This nursing care plan on sepsis provides a comprehensive approach to managing patients like Maria, who present with severe symptoms of sepsis. Sepsis, a critical condition requiring immediate attention, involves tailored nursing interventions and goals to ensure recovery.
Table of Contents: Nursing Care Plan on Sepsis
- Scenario
- Education for Patient and Family: Nursing Care Plan on Sepsis
- Comprehensive Assessment in the Nursing Care Plan on Sepsis
- Nursing Diagnoses in the Nursing Care Plan on Sepsis
- Goals for the Nursing Care Plan on Sepsis
- Nursing Interventions in the Nursing Care Plan on Sepsis
- Evaluation of the Nursing Care Plan on Sepsis
- References
You can
Scenario
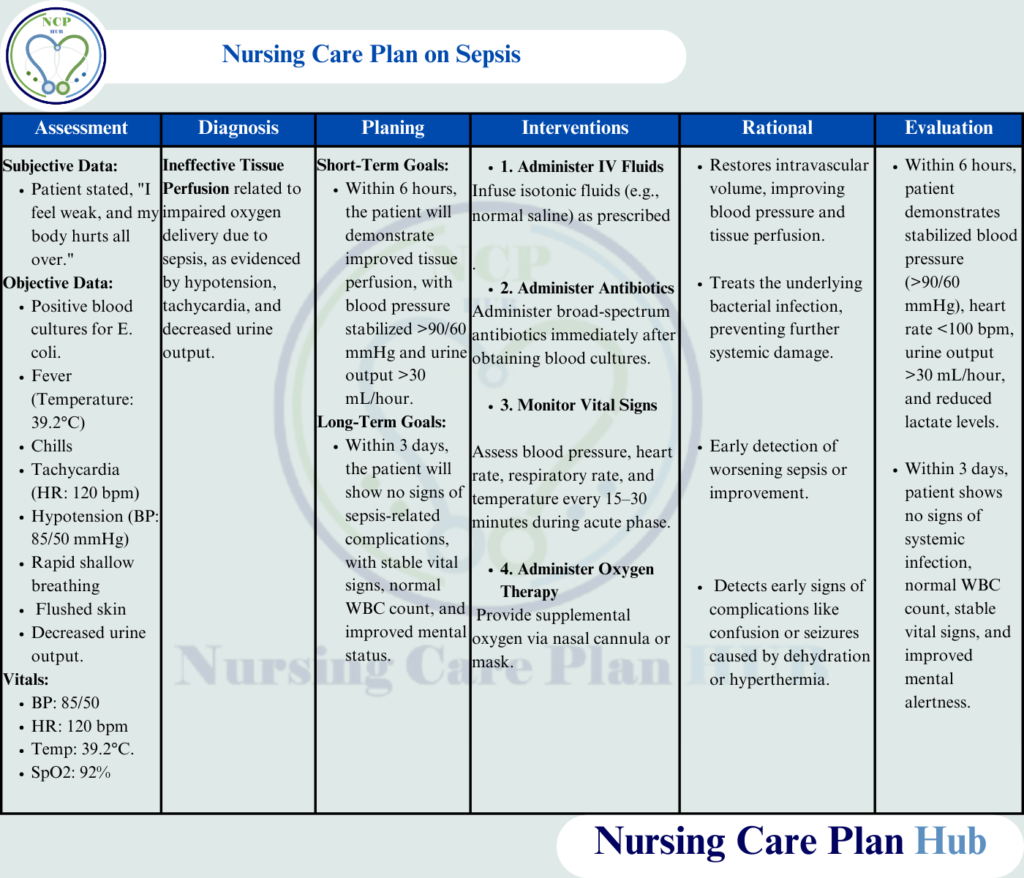
Patient Background: Maria, a 55-year-old female, is admitted to the hospital with fever, chills, and confusion. She reports a history of a recent urinary tract infection. Physical examination reveals hypotension (BP: 85/50 mmHg), tachycardia (HR: 120 bpm), fever (39.2°C), and tachypnea (RR: 26 breaths/min). Laboratory tests confirm elevated white blood cell count (WBC: 18,000/mm³), elevated lactate levels (4.0 mmol/L), and positive blood cultures for Escherichia coli.
Education for Patient and Family: Nursing Care Plan on Sepsis
Definition of Sepsis:
Sepsis is a life-threatening condition characterized by organ dysfunction resulting from the body’s dysregulated and overwhelming response to an infection. It is a medical emergency that requires prompt diagnosis and treatment to prevent complications. (World Health Organization, 2023).
Sepsis, also referred to as septicemia, is a life-threatening condition caused by an overwhelming response to infection. Early recognition and a detailed nursing care plan for septicemia are essential for effective treatment.
Pathophysiology:
When an infection occurs, the body activates its immune system to combat the invading microorganisms. In sepsis, this immune response becomes exaggerated and uncontrolled, causing widespread inflammation. This leads to increased capillary permeability, where fluid leaks from blood vessels into surrounding tissues, resulting in reduced blood flow and oxygen delivery to vital organs. As a result, multi-organ dysfunction or failure can occur if left untreated. (National Institutes of Health, 2023).
Causes:
Sepsis can arise from various infections, including:
- Bacterial infections such as pneumonia, urinary tract infections, or skin infections.
- Fungal or viral infections, including severe cases of influenza or COVID-19.
- Post-surgical complications due to infected wounds or invasive procedures.
Risk Factors:
Individuals at higher risk of developing sepsis include:
- Older adults (65 years and older).
- People with a weakened immune system (e.g., cancer patients or those on immunosuppressive therapy).
- Individuals with chronic illnesses like diabetes, chronic kidney disease, or heart disease.
- Patients who have undergone recent surgeries or prolonged hospitalization.
- People with invasive medical devices like catheters or breathing tubes.
Symptoms Identified in the Nursing Care Plan on Sepsis:
Early identification of sepsis is crucial. Common symptoms include:
- Fever (high temperature) or hypothermia (low temperature).
- Rapid heart rate (tachycardia).
- Increased breathing rate (tachypnea) or shortness of breath.
- Confusion, disorientation, or altered mental status.
- Low urine output, indicating kidney dysfunction.
- Low blood pressure, which can progress to septic shock.
Addressing these symptoms forms the foundation of any nursing care plan for patient with sepsis. Patients with conditions like diabetes or recent surgeries are at heightened risk, making nursing care for sepsis a priority in acute care settings.
Complications Addressed in the Nursing Care Plan on Sepsis:
Without prompt treatment, sepsis can lead to severe complications, including:
- Septic shock, characterized by dangerously low blood pressure and insufficient blood flow to vital organs.
- Acute Respiratory Distress Syndrome (ARDS), a severe lung condition causing respiratory failure.
- Kidney failure, requiring dialysis in some cases.
- Multi-organ dysfunction, where several organs like the heart, liver, and brain stop functioning properly.
- Death, in severe and untreated cases.
Also Read: Nursing Care Plan for Gastroenteritis
Comprehensive Assessment in the Nursing Care Plan on Sepsis
Monitor Vital Signs:
Frequent monitoring supports early detection of complications, aligning with sepsis nursing priorities and enabling timely interventions for patients in septic shock.
- What to Observe: Blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation.
- Rationale: Sepsis can progress rapidly to septic shock; frequent monitoring detects changes early.
- How to Perform: Use an automated monitor to check vitals hourly or as per protocol; ensure proper calibration of equipment.
Assess Neurological Status
Changes in mental status can guide nursing diagnosis for patient with sepsis, such as impaired cerebral perfusion.
- What to Check: Level of consciousness, confusion, or agitation.
- Rationale: Altered mental status indicates reduced cerebral perfusion due to systemic inflammation or hypoxia.
- How to Perform: Conduct a Glasgow Coma Scale (GCS) assessment every 2 hours and compare with baseline.
Monitor Fluid Balance
- What to Measure: Input (IV fluids, oral intake) and output (urine, vomitus, drains).
- Rationale: Fluid imbalances are common in sepsis due to increased vascular permeability.
- How to Perform: Use a Foley catheter for accurate urine measurement and record input/output every 4 hours.
Evaluate Skin and Peripheral Perfusion
- What to Look For: Cyanosis, mottling, pallor, or delayed capillary refill (>3 seconds).
- Rationale: These signs indicate reduced blood flow to peripheral tissues due to vasodilation and hypotension.
- How to Perform: Inspect extremities and perform capillary refill tests during every vital sign check.
Inspect for Infection Sources for Nursing Care Plan on Sepsis
Identifying infection sources is integral to both prevention and treatment, ensuring alignment with the nursing diagnosis related to sepsis and proper care plans.
- What to Check: Wounds, IV sites, surgical incisions, and devices (e.g., catheters, drains).
- Rationale: Identifying and managing infection sources prevents further spread.
- How to Perform: Use sterile gloves and appropriate lighting to examine potential infection sites.
Monitor Laboratory Results
- What to Observe: Lactate levels, WBC count, blood culture results, and organ function markers (e.g., creatinine, liver enzymes).
- Rationale: Elevated lactate and WBC levels are critical indicators of sepsis severity and guide treatment.
- How to Perform: Draw blood samples as per orders, ensure timely transport to the lab, and interpret results with the healthcare team.
Assess Respiratory Status
- What to Observe: Respiratory rate, depth, use of accessory muscles, and oxygen saturation.
- Rationale: Respiratory distress or ARDS is a common complication of sepsis.
- How to Perform: Conduct physical examination and auscultation every 4 hours or more frequently if respiratory distress occurs.
Assess Pain and Discomfort
- What to Check: Location, intensity, and nature of pain using a pain scale.
- Rationale: Pain is common due to inflammation or invasive procedures, and managing it can reduce stress.
- How to Perform: Use a numeric pain scale and provide interventions as prescribed.
Nursing Diagnoses in the Nursing Care Plan on Sepsis
For Maria, critical nursing diagnoses for septic shock include:
- Ineffective Tissue Perfusion related to systemic vasodilation and capillary leak syndrome, as evidenced by hypotension, tachycardia, and delayed capillary refill (NANDA International, 2023).
- Risk for Fluid Volume Deficit related to increased vascular permeability, fever, and reduced fluid intake (NANDA International, 2023).
Risk for Fluid Volume Deficit, a key consideration in any nursing care plan for septicemia.
Goals for the Nursing Care Plan on Sepsis
Setting specific nursing goals for sepsis helps ensure Maria’s recovery:
- Short-Term Goal: Within 12 hours, Maria will demonstrate improved tissue perfusion as evidenced by stabilized blood pressure, improved mental status, and normal capillary refill.
- Long-Term Goal: Within 5 days, Maria will remain hemodynamically stable, maintain organ function, and understand sepsis prevention measures.
Nursing Interventions in the Nursing Care Plan on Sepsis
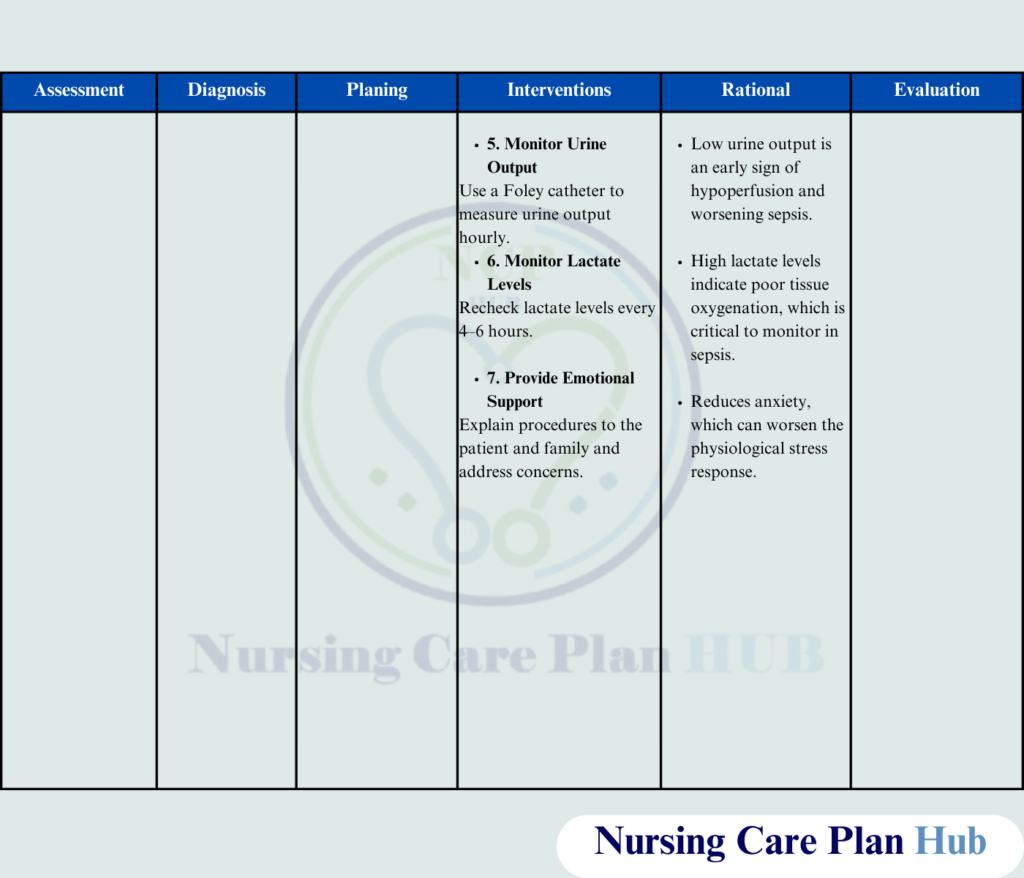
Effective nursing interventions for sepsis patient care include:
Administer IV Fluids as Prescribed:
Restores perfusion and supports nursing dx for sepsis.
- Rationale: Restores intravascular volume, improves cardiac output, and enhances tissue perfusion.
- How to Perform: Administer isotonic solutions (e.g., normal saline or Ringer’s lactate) using an infusion pump; monitor for signs of fluid overload.
Administer Broad-Spectrum Antibiotics
- Rationale: Early antibiotic therapy targets the infection source, preventing further systemic spread.
- How to Perform: Administer within 1 hour of sepsis diagnosis; check allergies before administration.
Provide Oxygen Therapy
- Rationale: Maintains oxygenation and prevents hypoxia caused by impaired perfusion.
- How to Perform: Apply nasal cannula or mask as needed; titrate flow rate to keep oxygen saturation above 94%.
Monitor and Manage Fever
- Rationale: Reducing fever minimizes metabolic demand and improves patient comfort.
- How to Perform: Administer antipyretics like acetaminophen and use cooling blankets if needed.
Collaborate for Source Control
- Rationale: Removing or treating the source of infection halts the progression of sepsis.
- How to Perform: Prepare for procedures like catheter removal or abscess drainage in collaboration with the medical team.
Administer Vasopressors if Indicated
- Rationale: Vasopressors like norepinephrine stabilize blood pressure in cases of septic shock.
- How to Perform: Administer via a central line with continuous blood pressure monitoring.
Monitor Blood Glucose Levels
- Rationale: Hyperglycemia can worsen inflammation and sepsis progression.
- How to Perform: Check blood glucose levels every 4–6 hours and administer insulin as prescribed.
Educate the Patient and Family About Sepsis
- Rationale: Increases awareness and enables early recognition of infection signs.
- How to Perform: Explain infection prevention strategies, importance of completing antibiotics, and when to seek medical attention.
Evaluation of the Nursing Care Plan on Sepsis
Using this detailed care plan for sepsis, Maria demonstrated improved vital signs, normalized laboratory values, and an understanding of preventive measures, meeting the established nursing goals for sepsis.
- Tissue Perfusion: Maria’s blood pressure stabilized (BP: 110/70 mmHg), capillary refill <2 seconds, and mental status returned to baseline.
- Fluid Balance: Adequate urine output (>0.5 mL/kg/hour) with no signs of dehydration or overload.
- Infection Control: WBC count returned to normal levels, and blood cultures were negative after completing antibiotics.
- Patient Understanding: Maria and her family verbalized understanding of sepsis prevention and early detection strategies.
Here you can download the PDF file of nursing care plan for Sepsis
References
- Centers for Disease Control and Prevention. (2023). Sepsis: Symptoms, prevention, and treatment.
- NANDA International. (2023). NANDA-I nursing diagnoses: Definitions & classification 2023-2025.
- National Institutes of Health. (2023). Sepsis and septic shock: Pathophysiology and management.
- World Health Organization. (2023). Global guidelines for the prevention and treatment of sepsis.

Excellent Work 💯👏
Highly Recommended