Insomnia is a common sleep disorder that affects a person’s ability to fall or stay asleep, leading to daytime fatigue, irritability, and decreased productivity. A well-structured nursing care plan on insomnia focuses on identifying the underlying causes, such as poor sleep hygiene, stress, or irregular sleep schedules, and implementing effective insomnia interventions nursing to improve the patient’s sleep quality. By addressing specific factors and creating an individualized insomnia NCP, nurses can help patients achieve restful sleep, reduce complications, and enhance their overall well-being.
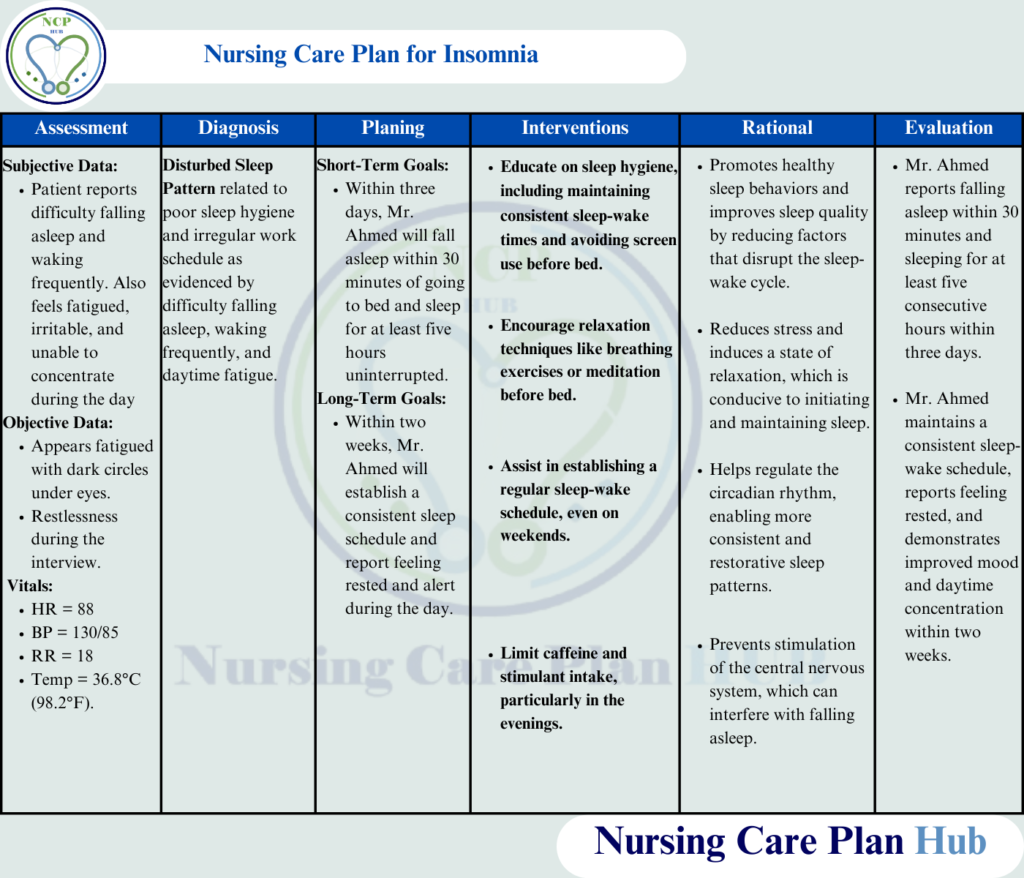
Nursing Care Plan on Insomnia in picture form is given below to help students:
You can
Scenario
Patient Background:
Mr. Ahmed, a 45-year-old office worker, presents to the outpatient clinic with complaints of difficulty falling asleep and staying asleep for the past three months. He reports feeling tired during the day, difficulty concentrating, and irritability. His work involves late-night shifts, and he often consumes coffee in the evening. He has tried over-the-counter sleep aids without success and feels his sleep pattern has significantly impacted his daily life.
Education for Patient
Educating patients about sleep hygiene is a vital component of a nursing care plan for sleep.
What is Insomnia?
Insomnia is a sleep disorder characterized by difficulty initiating or maintaining sleep, or waking up too early and being unable to return to sleep, despite having sufficient time and opportunity for rest. This persistent lack of restful sleep leads to daytime fatigue, irritability, and impaired functioning. According to the World Health Organization (2023), insomnia is a common issue worldwide that significantly impacts mental and physical health.
Pathophysiology:
Insomnia is often linked to a state of hyperarousal, which results from stress and disruptions in the body’s natural sleep-wake cycle. Chronic activation of the hypothalamic-pituitary-adrenal (HPA) axis leads to elevated cortisol levels, impairing the body’s ability to fall asleep and stay asleep. The National Institutes of Health (2023) explains that this prolonged stress response exacerbates sleep difficulties, creating a cycle that makes insomnia harder to manage.
Causes:
To develop an effective nursing care plan on insomnia, understanding the underlying causes is crucial.
- Stress: Emotional stress from life events or psychological issues can trigger insomnia.
- Irregular Sleep Patterns: Frequent changes in sleep schedules, such as shift work, disrupt the body’s circadian rhythm.
- Substance Use: Excessive consumption of caffeine, alcohol, or nicotine affects the sleep cycle.
- Medical Conditions: Anxiety, depression, chronic pain, and conditions like restless leg syndrome can all contribute to sleep disturbances.
- Poor Sleep Hygiene: Factors such as an uncomfortable sleep environment or the use of electronic devices before bed can hinder the ability to fall asleep. (American Sleep Association, 2023)
Risk Factors:
- Shift work
- Chronic stress
- Advanced age
- Psychiatric disorders (e.g., anxiety, depression)
- Substance abuse (e.g., caffeine, alcohol, nicotine)
- Poor sleep hygiene
Symptoms:
Symptoms of insomnia can vary in severity but commonly include:
- Difficulty falling asleep
- Frequent wake-ups during the night
- Early morning waking and inability to fall back asleep
- Fatigue or feeling unrested despite adequate time in bed
- Mood disturbances (irritability, anxiety, depression)
- Cognitive impairment (difficulty concentrating, poor memory)
- Decreased daytime functioning (impaired performance at work or school) (National Institutes of Health, 2023)
Complications:
If left untreated, insomnia can lead to serious health complications, including:
- Increased risk of depression and anxiety
- Higher likelihood of developing cardiovascular diseases (e.g., hypertension, heart disease)
- Impaired immune system function
- Cognitive decline (poor memory, decision-making abilities)
- Decreased quality of life due to chronic fatigue
Also Read: Nursing Care Plan for Impaired Gas Exchange
Comprehensive Assessment
1. History
- Rationale: Gathering detailed history aids in understanding the onset, duration, and triggers of insomnia (American Sleep Association, 2023).
- Assessment:
- Difficulty falling asleep and staying asleep for the past three months.
- Reports feeling fatigued, irritable, and unable to concentrate during the day (World Health Organization, 2023).
- Work schedule involves late-night shifts, contributing to irregular sleep patterns (National Institutes of Health, 2023).
- Regular evening consumption of coffee.
- Tried over-the-counter sleep aids without success.
2. General Assessment and Motor Behavior
- Rationale: Physical appearance and activity level may provide clues about the impact of sleep deprivation (American Sleep Association, 2023).
- Assessment:
- Appears fatigued, with dark circles under eyes.
- Exhibits restlessness during the interview.
3. Mood and Affect
- Rationale: Insomnia often coexists with mood disturbances, such as anxiety and depression (World Health Organization, 2023).
- Assessment:
- Mood: Reports feeling frustrated and anxious about his sleep difficulties.
- Affect: Congruent with mood, appears irritable and easily frustrated.
4. Thought Process and Content
- Rationale: Identifying cognitive distortions or sleep-related anxiety is crucial for understanding the psychological impact of insomnia (National Institutes of Health, 2023).
- Assessment:
- Thought process: Logical and coherent.
- Content: Preoccupied with concerns about the inability to sleep and its impact on his performance at work.
5. Sensorium and Intellectual Processes
- Rationale: Chronic insomnia may affect cognitive functions like memory and concentration (American Sleep Association, 2023).
- Assessment:
- Oriented to time, place, and person.
- Reports mild difficulty concentrating during work tasks.
6. Abnormal Sensory Experiences
- Rationale: Sleep deprivation may result in perceptual disturbances, such as hallucinations or misperceptions (National Institutes of Health, 2023).
- Assessment:
- No reports of hallucinations or perceptual abnormalities.
7. Judgment and Insight
- Rationale: Understanding of the problem and decision-making abilities are essential for planning care (World Health Organization, 2023).
- Assessment:
- Judgment: Adequate, seeks medical intervention.
- Insight: Partial; understands the impact of coffee and work schedule but struggles to implement changes.
8. Self-Concept
- Rationale: Insomnia may affect self-esteem and self-perception, leading to reduced confidence (National Institutes of Health, 2023).
- Assessment:
- Reports feeling inadequate at work due to reduced productivity and irritability.
9. Role and Relationships
- Rationale: Assessing interpersonal dynamics highlights the broader impact of insomnia on personal and professional relationships (World Health Organization, 2023).
- Assessment:
- Strained relationships with colleagues due to irritability.
- Limited interaction with family due to late-night shifts and daytime fatigue.
10. Physiological and Self-Care Considerations
- Rationale: Insomnia often affects physical health and daily functioning, leading to chronic fatigue and somatic symptoms (American Sleep Association, 2023).
- Assessment:
- Reports daytime fatigue, reduced appetite, and occasional headaches.
- Irregular sleep schedule due to work demands.
- No significant weight changes or chronic medical conditions reported.
Nursing Diagnoses
Insomnia related to nursing diagnosis includes factors such as poor sleep hygiene and anxiety.
- Disturbed Sleep Pattern related to poor sleep hygiene and lifestyle factors as evidenced by difficulty falling asleep, waking frequently, and feeling fatigued during the day (NANDA International, 2023).
- Fatigue related to chronic sleep deprivation as evidenced by daytime tiredness, irritability, and impaired concentration (NANDA International, 2023).
Planning & Goals
The primary objective of this insomnia NCP is to establish a regular sleep pattern and improve sleep quality.
Short-Term Goals for Nursing Care Plan on Insomnia:
Within three days, Mr. Ahmed will report falling asleep within 30 minutes of going to bed and sleeping for at least five consecutive hours.
Long-Term Goal for Nursing Care Plan on Insomnia:
Within two weeks, Mr. Ahmed will establish a consistent sleep schedule and report feeling rested and alert during the day.
Nursing Interventions with Rationale
Sleep nursing care plans for insomnia often include relaxation techniques to reduce hyperarousal and improve sleep latency
Educate on Sleep Hygiene
Rationale: Maintaining a consistent bedtime, limiting caffeine, and creating a relaxing pre-sleep routine improve sleep quality (American Sleep Association, 2023).
How to Perform: Provide written guidelines on sleep hygiene and discuss changes like avoiding screen time and reducing stimulants in the evening.
Encourage the Use of Relaxation Techniques
Rationale: Practices such as progressive muscle relaxation or meditation reduce stress and promote sleep (World Health Organization, 2023).
How to Perform: Teach Mr. Ahmed simple breathing exercises or guided imagery to use before bedtime.
Establish a Regular Sleep-Wake Schedule
Rationale: Consistency helps regulate the circadian rhythm, improving sleep quality (National Institutes of Health, 2023).
How to Perform: Assist Mr. Ahmed in creating a bedtime and wake-up time that suits his lifestyle and encourage adherence even on weekends.
Limit Stimulant Intake
Rationale: Reducing caffeine and alcohol consumption prevents stimulation of the central nervous system (American Sleep Association, 2023).
How to Perform: Provide dietary counseling, highlighting the effects of stimulants on sleep and suggesting herbal teas or decaffeinated beverages.
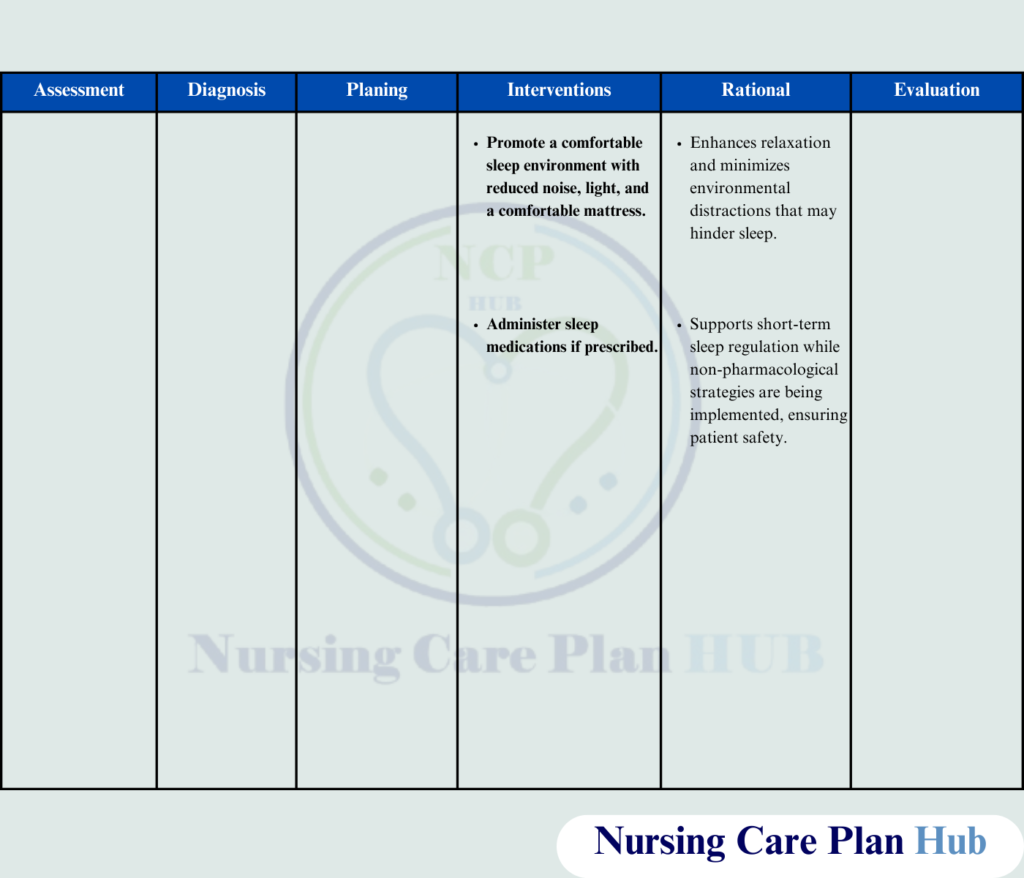
Provide Cognitive Behavioral Therapy for Insomnia (CBT-I)
Rationale: CBT-I addresses negative thoughts and behaviors associated with insomnia and has long-term efficacy (National Institutes of Health, 2023).
How to Perform: Refer to a trained therapist or provide resources for online CBT-I programs.
Administer Sleep Medications if Prescribed
Rationale: Short-term use of hypnotics may help re-establish sleep patterns while implementing behavioral changes (World Health Organization, 2023).
How to Perform: Monitor Mr. Ahmed for side effects and ensure he understands the short-term nature of medication use.
Promote a Comfortable Sleep Environment
Rationale: Reducing noise, light, and ensuring a comfortable mattress promote restful sleep (American Sleep Association, 2023).
How to Perform: Advise Mr. Ahmed to adjust his sleeping area, including blackout curtains and white noise machines, if necessary.
Here you can download the PDF file of nursing care plan for sleep.
Evaluation
Evaluation of the insomnia interventions nursing shows improved patient sleep patterns and reduced fatigue
- Improved Sleep: Mr. Ahmed reports falling asleep within 30 minutes and sleeping for six uninterrupted hours.
- Increased Daytime Energy: Mr. Ahmed reports feeling less fatigued and demonstrates improved concentration and mood.
- Knowledge Retention: Mr. Ahmed successfully adheres to his sleep schedule and relaxation techniques.
References
- American Sleep Association. (2023). Insomnia: Causes, symptoms, and treatment.
- NANDA International. (2023). NANDA-I nursing diagnoses: Definitions & classification 2023-2025.
- National Institutes of Health. (2023). Sleep disorders and management guidelines.
- World Health Organization. (2023). Sleep health and interventions for better outcomes.
love to read this