This guide provides a detailed nursing care plan on fever, covering common conditions such as pyrexia, hyperpyrexia, and viral fever. Understanding the nursing diagnosis related to fever helps in crafting effective interventions to manage high temperatures.
Table of Content:
- Patient Scenario: Nursing Care Plan for Fever Due to Pneumonia
- Education For Patient on Fever
- Comprehensive Patient Assessment
- NANDA Nursing Diagnosis for Fever and Pyrexia
- Planning
- Nursing Interventions for Fever: Step-by-Step Guide
- Nursing Process for Fever: Evaluation
- Comprehensive Nursing Care for Fever Patients
You can Downlaod the nursing care plan for Pyrexia in
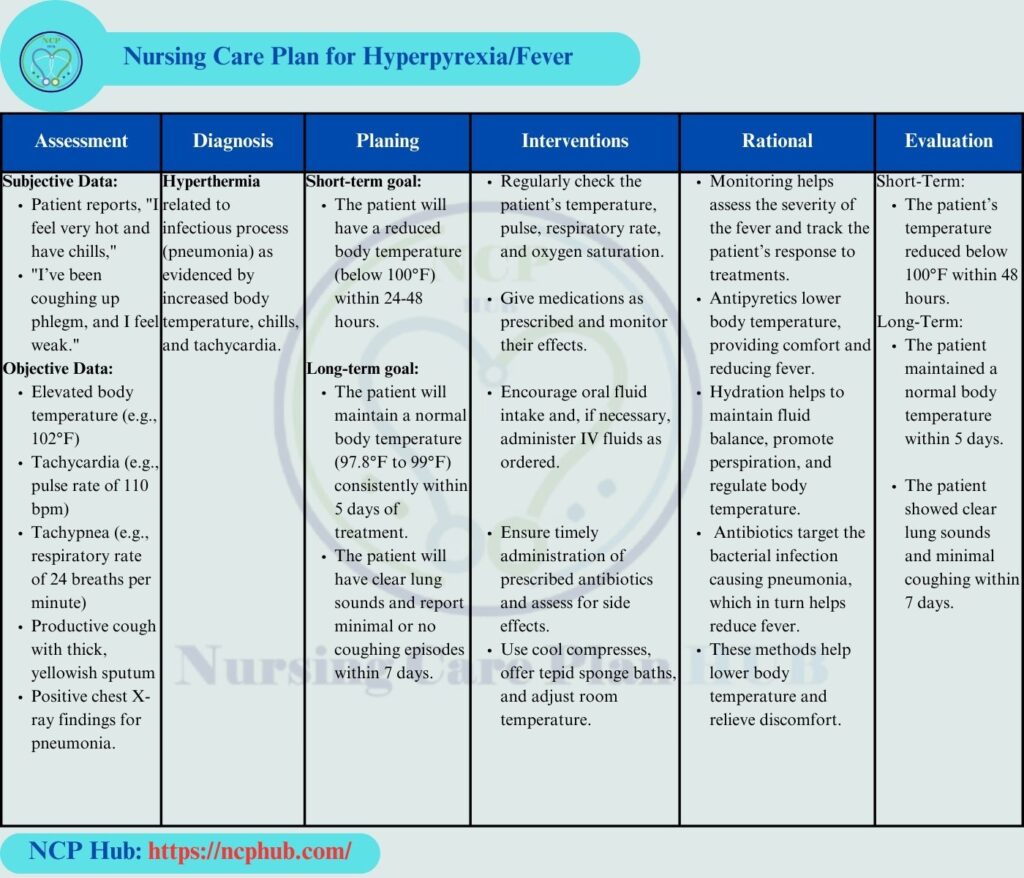
Patient Scenario: Nursing Care Plan for Fever Due to Pneumonia
In this ncp on fever, we address the case of Mr. Ahmed, a 45-year-old patient presenting with a high-grade fever (pyrexia) due to pneumonia. Understanding the nursing process for fever, including a thorough assessment and tailored interventions, is essential for effective patient care.
Patient: Mr. Ahmed
Age: 45 years
Presenting Condition: Mr. Ahmed presents to the emergency department with a high-grade fever of 102°F (38.9°C), productive cough with yellow sputum, chest discomfort, and shortness of breath. He reports that his fever has persisted for three days, accompanied by fatigue and chills. His medical history includes well-controlled hypertension.

Education For Patient on Fever
Definition:
Fever is an increase in body temperature above the normal range, typically defined as exceeding 100.4°F (38°C). It is commonly a symptom of an underlying infection or inflammatory process.
Reference: McNaughton, J. R. (2017). Pathophysiology Made Incredibly Easy!.
Fever, or hyperpyrexia, is an elevated body temperature often linked to underlying infections like pneumonia. The nursing diagnosis for fever according to NANDA focuses on identifying the root causes and formulating a careplan for fever to manage symptoms effectively. Fever can be a result of bacterial infections, and a comprehensive nursing care plan for pyrexia will help in addressing the patient’s needs.
Pathophysiology:
Fever occurs when pyrogens (substances that induce fever) trigger the hypothalamus to elevate the body’s temperature set point. This response is part of the immune system’s effort to combat infections, enhancing the activity of immune cells and inhibiting pathogen growth.
Reference: Kuhlman, K. (2020). Fever: Pathophysiology and Treatment. American Family Physician, 102(1), 24-30.
Causes of Fever:
- Infections: Bacterial (e.g., pneumonia), viral, or fungal infections.
- Reference: Steer, A. C., & Hodge, N. (2016). Fever in Children: Diagnosis and Management. BMJ, 353, i2025.
Risk Factors:
- Age: Infants and the elderly are more vulnerable.
- Existing Health Conditions: Individuals with compromised immune systems are at greater risk.
Reference: Ader, R. (2019). Factors that Influence the Severity of Fever. Journal of Clinical Medicine, 8(4), 546.
Complications:
- Dehydration: Increased fluid loss can lead to severe dehydration.
- Febrile Seizures: Particularly in children, high fever may trigger seizures.
- Worsening of Underlying Conditions: Chronic diseases may exacerbate without timely treatment.
Reference: Afolabi, M. O., & Adebayo, A. M. (2021). Complications of Fever: A Review of Recent Literature. Nigerian Journal of Clinical Practice, 24(2), 137-143.
Comprehensive Patient Assessment
Vital Signs
- Intervention: Monitor vital signs every 2 hours.
- Rationale: Continuous monitoring allows for timely identification of changes in Mr. Ahmed’s condition, facilitating prompt interventions.
- How to Perform: Use an electronic thermometer to measure body temperature, noting any changes. Assess heart rate, respiratory rate, blood pressure, and oxygen saturation with a pulse oximeter, documenting each reading in the patient’s chart.
Respiratory Assessment:
- Intervention: Auscultate lung sounds.
- Rationale: This helps identify any abnormalities such as wheezing or crackles, which are common in pneumonia.
- How to Perform: Place the stethoscope on the chest and back while instructing Mr. Ahmed to take deep breaths. Document the presence of any abnormal sounds.
General Appearance:
- Intervention: Observe Mr. Ahmed’s general appearance.
- Rationale: Signs of distress, lethargy, or dehydration can indicate the severity of the illness.
- How to Perform: Assess his ability to respond to questions and his level of alertness, noting any signs of fatigue or discomfort.
Skin Assessment:
- Intervention: Check skin turgor and moisture.
- Rationale: Adequate skin turgor is indicative of hydration status.
- How to Perform: Pinch the skin on the back of the hand and observe for elasticity. Assess for diaphoresis (sweating) or dry skin.
Neurological Assessment:
- Intervention: Evaluate orientation and level of consciousness.
- Rationale: Altered mental status can indicate severe infection or systemic response.
- How to Perform: Ask Mr. Ahmed simple questions such as his name, where he is, and what day it is. Document his responses.
Exceptional Cases:
If Mr. Ahmed exhibits altered mental status, hypotension, or severe respiratory distress, I will notify the physician immediately and take appropriate emergency measures.
Reference: McCance, K. L., & Huether, S. E. (2019). Pathophysiology: The Biologic Basis for Disease in Adults and Children (8th ed.). Elsevier.
NANDA Nursing Diagnosis for Fever and Pyrexia
Diagnoses:
- Hyperthermia related to infection (pneumonia) as evidenced by elevated temperature of 103°F, chills, and fatigue.
- Impaired gas exchange related to lung infection as evidenced by shortness of breath and O2 saturation of 93% on room air.
How to Formulate the Diagnoses:
- I used the statement “Hyperthermia related to infection” because the elevated temperature indicates an ongoing immune response to pneumonia. The supporting evidence includes the high fever and associated symptoms like chills.
- For the second diagnosis, I formulated “Impaired gas exchange related to lung infection” based on the observed shortness of breath and low oxygen saturation, indicating respiratory compromise.
Prioritization of Diagnoses:
- The diagnosis of hyperthermia is prioritized because it poses an immediate risk to Mr. Ahmed’s health and requires prompt intervention to prevent complications.
- The impaired gas exchange diagnosis is also critical, as it directly affects oxygenation and overall respiratory function.
Reference: North American Nursing Diagnosis Association (NANDA). (2018). Nursing Diagnoses Definitions and Classification 2018-2020.
Planning
Goals and Nursing Interventions for Fever
Effective nursing care for a patient with fever should aim to:
- Reduce the fever (temperature below 100°F).
- Maintain adequate hydration.
- Ensure proper oxygenation for patients with respiratory conditions like pneumonia.
Prioritization of Goals:
- The primary focus is on reducing Mr. Ahmed’s fever and ensuring adequate oxygenation, as these are critical to his immediate health and recovery.

Nursing Interventions for Fever: Step-by-Step Guide
Nursing interventions for fever include monitoring vital signs, administering antipyretics, and encouraging fluid intake. The careplan for fever should also involve education on fever and its complications.
Monitoring Vital Signs
- Intervention: Monitor vital signs every 2 hours.
- Rationale: Continuous monitoring allows for timely identification of changes in Mr. Ahmed’s condition, facilitating prompt interventions.
- How to Perform: Regularly check temperature, heart rate, respiratory rate, and oxygen saturation, documenting each in the medical record. This will help in determining the effectiveness of interventions and the patient’s response.
Administering Antipyretics
- Intervention: Administer acetaminophen as prescribed.
- Rationale: Antipyretics help reduce fever and alleviate discomfort.
- How to Perform: Administer the medication orally or via IV as prescribed. Monitor for adverse reactions and reassess temperature after two hours. Prioritizing this intervention is crucial because fever reduction is essential to improve comfort and facilitate recovery.
Encouraging Fluid Intake
- Intervention: Encourage oral fluid intake of at least 2-3 liters per day.
- Rationale: Maintaining hydration is essential to prevent dehydration and support the immune response.
- How to Perform: Offer water and electrolyte solutions frequently, documenting intake and assessing for signs of dehydration. This intervention is prioritized to support kidney function and overall recovery.
Administering Antibiotics
- Intervention: Administer prescribed broad-spectrum antibiotics.
- Rationale: Antibiotics are crucial for eradicating the bacterial infection causing pneumonia.
- How to Perform: Administer the medication via IV, observing for allergic reactions, and document the administration. Prompt antibiotic therapy is prioritized to combat the infection quickly and effectively.
Providing Oxygen Therapy
- Intervention: Administer oxygen via nasal cannula.
- Rationale: Supplemental oxygen helps improve oxygenation in patients with impaired gas exchange.
- How to Perform: Attach a nasal cannula and set the flow rate to 2 L/min. Monitor O2 saturation continuously. Prioritizing this intervention is critical to ensure adequate oxygen delivery to tissues.
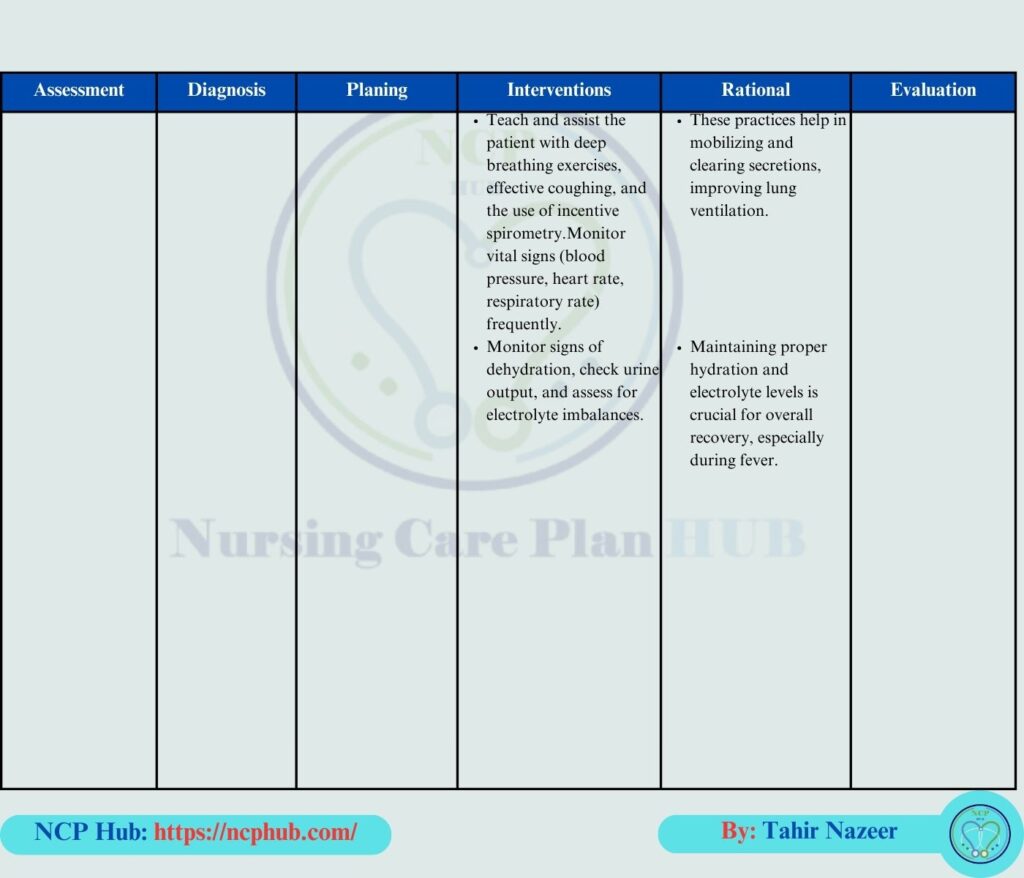
Encouraging Deep Breathing and Coughing
- Intervention: Teach and encourage deep breathing and coughing exercises.
- Rationale: These exercises help clear secretions and improve lung function.
- How to Perform: Demonstrate the techniques, guiding Mr. Ahmed to perform them every hour. Document his participation and any difficulty experienced. This intervention is prioritized as it directly supports respiratory function and reduces the risk of atelectasis.
Nursing Process for Fever: Evaluation
Goal 1: Assess temperature every 2 hours. If Mr. Ahmed’s temperature is below 100°F after interventions, the goal is met. If not, reassess the interventions and consult with the healthcare provider for further actions.
Goal 2: Monitor O2 saturation continuously. If O2 saturation is above 95% within 48 hours, the goal is met. If not, additional interventions may be required, such as increasing oxygen flow or administering bronchodilators.
Goal 3: Assess Mr. Ahmed’s report of fatigue and chest discomfort. If he reports significant improvement within 48 hours, the goal is met. If symptoms persist, review and adjust the care plan as necessary.
For a downloadable version of this plan, see our nursing care plan for fever PDF.
Comprehensive Nursing Care for Fever Patients
From nursing care for patients with fever to handling fever NANDA nursing diagnoses, understanding how to manage high temperatures and related symptoms is crucial. This fever nursing care plan PDF offers detailed guidelines and actionable steps for healthcare professionals.

Keep it up 💪
Hello.
Good cheer to all on this beautiful day!!!!!
Good luck 🙂
Amazing
You’ve the most impressive websites.