Pressure ulcers, commonly known as bed sores, are a critical concern in healthcare settings, especially for patients with limited mobility. Developing an effective nursing care plan for impaired skin integrity is essential for promoting healing and preventing complications.
You can
NCP on Pressure Ulcer
Scenario
John, a 75-year-old male, is bedridden after a recent hip fracture surgery. Due to prolonged immobility, he has developed a stage II pressure ulcer on his sacral region. The ulcer measures 3 cm in diameter, with visible redness, partial skin loss, and mild drainage. His skin is fragile, and his nutritional intake has been insufficient due to poor appetite. John’s physician has prescribed wound care, repositioning, and nutritional support to manage the pressure ulcer. John’s condition requires a detailed care plan for impaired skin integrity to address the stage II pressure ulcer effectively.
Education for Patient
Educating patients and caregivers about the risk for impaired skin integrity is crucial. Understanding the causes and symptoms can aid in implementing preventive measures, especially in those at high risk for developing pressure ulcers.
What is Pressure Ulcer or Bed Sore?
According to the World Health Organization (WHO), a pressure ulcer, also known as a bed sore, is a localized injury to the skin and/or underlying tissue, usually over a bony prominence, due to prolonged pressure (World Health Organization, 2023).
Pathophisiology
Pressure ulcers form when blood flow is restricted due to constant pressure, leading to tissue ischemia, cell death, and ulcer formation. According to the National Institutes of Health (NIH), immobility and pressure exerted over bony areas reduce blood flow, causing cell damage and skin breakdown (National Institutes of Health, 2023).
Causes
Primary causes include prolonged immobility, friction, shear, and inadequate nutrition, all of which compromise skin integrity and delay healing (American Academy of Dermatology, 2022).
Risk Factors
Factors increasing the risk for bed sores include advanced age, limited mobility, incontinence, poor nutrition, and chronic health conditions like diabetes (World Health Organization, 2023).
Symptoms
Redness, pain, skin breakdown, partial or complete skin loss, and, in advanced cases, exposure of underlying tissues (National Institutes of Health, 2023).
Complications
Untreated pressure ulcers can lead to infections, osteomyelitis (bone infection), sepsis, and delayed wound healing (American Academy of Dermatology, 2022).
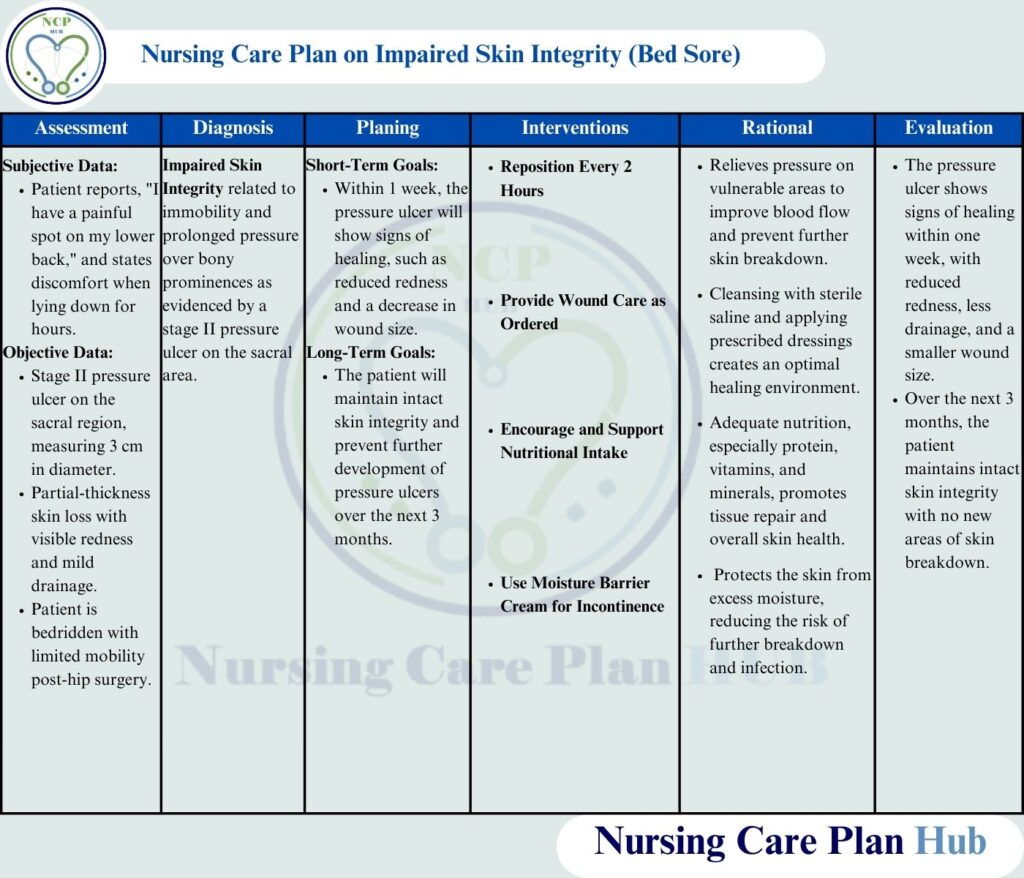
Assessment
Nursing Care Plan for Impaired Skin Integrity needs a comprihensve assessment systematically to achieve outcomes.
Assess Skin Integrity
Rationale: Conducting a thorough assessment is the first step in creating a nursing care plan for impaired skin integrity. This helps identify early signs of breakdown and tailor interventions accordingly
How to Perform: Inspect skin daily, especially over bony prominences. Document any changes in color, texture, or integrity, and measure wound size, depth, and any exudate.
Evaluate Nutritional Status
Rationale: Malnutrition delays wound healing by limiting necessary nutrients needed for tissue repair (American Society for Parenteral and Enteral Nutrition, 2022).
How to Perform: Conduct a dietary assessment by reviewing John’s meal intake and weight history. Collaborate with a dietitian to create a nutrition plan rich in protein, vitamins, and minerals.
Assess for Pain and Discomfort
Rationale: Addressing pain is a crucial component of impaired skin integrity nursing interventions and rationales. Effective pain management improves compliance with necessary repositioning. (American Academy of Dermatology, 2022).
How to Perform: Use a pain scale (0–10) to assess discomfort levels, especially when repositioning or providing wound care.
Monitor for Signs of Infection
Rationale: Pressure ulcers are susceptible to infection, which can complicate healing and spread to other areas (National Institutes of Health, 2023).
How to Perform: Check for increased redness, warmth, swelling, odor, or purulent discharge around the wound, and report any abnormalities to the physician.
Assess Mobility and Repositioning Needs
Rationale: Repositioning relieves pressure, reducing the risk of further skin breakdown (National Pressure Ulcer Advisory Panel, 2023).
How to Perform: Evaluate John’s ability to reposition himself and provide assistance as needed. Use positioning devices, such as foam cushions or wedges, to offload pressure from the affected area.
Evaluate Continence and Hygiene Needs
Rationale: Incontinence can increase skin moisture, contributing to skin breakdown (American Geriatrics Society, 2023).
How to Perform: Assess John’s continence status and, if needed, use moisture barriers and frequent hygiene practices to keep the skin dry and intact.
Also Read: Nursing Care Plan on Hypokalemia
Nursing Diagnoses
John’s condition aligns with the nursing diagnosis of impaired skin integrity due to immobility and pressure on bony prominences.
- Impaired Skin Integrity related to immobility and pressure over bony prominences secondary to stage II pressure ulcer as evidenced by partial skin loss and redness over the sacral area (NANDA International, 2023).
- Risk for Infection related to open wound secondary to pressure ulcer as evidenced by partial skin loss and drainage (NANDA International, 2023).
A well-structured impaired skin integrity NCP (nursing care plan) is vital for patients at risk of pressure ulcers
Goals of Nursing Care Plan for Impaired Skin Integrity
Short-Term Goal:
Within 1 week, John’s pressure ulcer will show signs of healing, achieving a primary nursing outcome for impaired skin integrity by reducing redness and wound size
Within 1 week, John’s pressure ulcer will show signs of healing, including reduced redness and a smaller wound size, with no additional areas of skin breakdown (American Academy of Dermatology, 2022).
Long-Term Goal:
John will maintain intact skin integrity and prevent further development of pressure ulcers by adhering to a repositioning schedule and skin care regimen over the next three months (National Pressure Ulcer Advisory Panel, 2023).
Nursing Interventions
Reposition Every 2 Hours
Rationale: Repositioning helps relieve pressure on areas vulnerable to skin breakdown (National Pressure Ulcer Advisory Panel, 2023).
How to Perform: Assist John in changing positions at least every 2 hours. Use pillows or foam padding to support different body parts, avoiding pressure on the sacral area.
Provide Wound Care as Ordered
Rationale: Proper wound care prevents infection and promotes healing by creating a clean, moist wound environment (American Academy of Dermatology, 2022).
How to Perform: Cleanse the wound with a sterile saline solution, apply prescribed dressings, and ensure dressing changes are completed according to orders.
Encourage and Support Nutritional Intake
Rationale: Adequate nutrition, especially with protein, vitamins A and C, and zinc, supports skin repair and immune function (American Society for Parenteral and Enteral Nutrition, 2022).
How to Perform: Provide protein-rich meals and snacks, and collaborate with a dietitian to develop a meal plan that addresses John’s nutritional needs. Encourage small, frequent meals if appetite is limited.
Use Moisture Barrier Cream for Incontinence
Rationale: Moisture barriers protect the skin from excess moisture, which can lead to breakdown and infection (American Geriatrics Society, 2023).
How to Perform: After each incontinence episode, cleanse John’s skin with a gentle cleanser, dry thoroughly, and apply a moisture barrier cream to prevent skin breakdown.
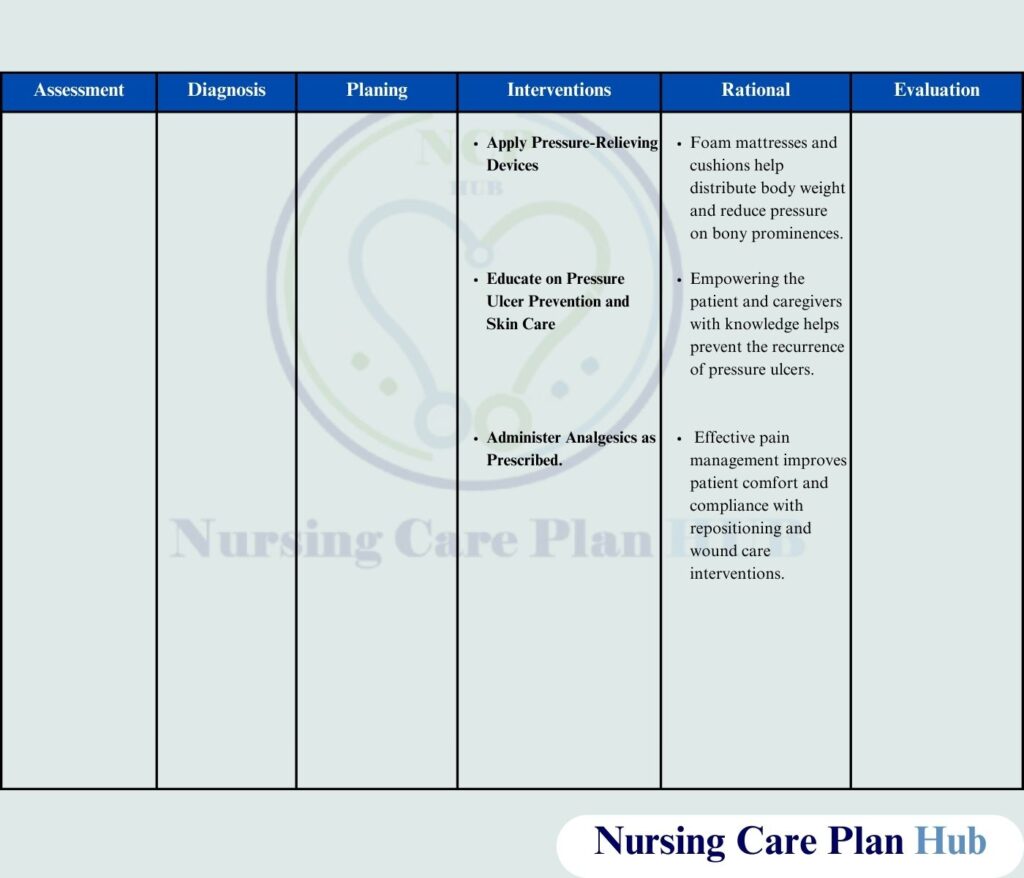
Apply Pressure-Relieving Devices
Rationale: Devices such as foam mattresses and cushions distribute body weight evenly, reducing pressure on bony prominences (National Pressure Ulcer Advisory Panel, 2023).
How to Perform: Position cushions under John’s legs and back to elevate pressure-prone areas off the bed surface.
Educate on Pressure Ulcer Prevention and Skin Care
Rationale: Understanding how to manage pressure ulcers empowers John and his caregivers to actively participate in his care, reducing the risk of further skin breakdown (World Health Organization, 2023).
How to Perform: Explain the importance of repositioning, using supportive surfaces, and keeping the skin clean and dry. Provide written materials and demonstration as needed.
Administer Analgesics as Prescribed
Rationale: Pain relief is necessary to improve comfort and compliance with necessary interventions, such as repositioning (National Institutes of Health, 2023).
How to Perform: Administer analgesics 30 minutes before any movement or wound care, as prescribed, and assess for pain relief effectiveness.
Evaluation
Regular evaluation of John’s progress will determine the effectiveness of the NCP for skin integrity, ensuring no new pressure ulcers develop.
- Wound Healing Progress: The pressure ulcer shows signs of healing, with reduced redness, drainage, and decreased size.
- Symptom Management: John reports reduced pain during repositioning and wound care, indicating effective pain management.
- Improved Skin Integrity: No new areas of skin breakdown are observed, and John’s skin remains intact.
- Patient and Caregiver Knowledge: John and his caregivers demonstrate understanding of preventive measures and perform skin care interventions appropriately.
Implementing a comprehensive nursing care plan for impaired skin integrity is vital for patients like John. By following the outlined interventions, healthcare professionals can improve patient outcomes and prevent complications associated with pressure ulcers.
Here you can download the pdf file of ncp on bed sore
References
- American Academy of Dermatology. (2022). Skin integrity and wound care management. American Academy of Dermatology.
- American Geriatrics Society. (2023). Incontinence and skin care recommendations. American Geriatrics Society.
- American Society for Parenteral and Enteral Nutrition. (2022). Nutritional guidelines for wound healing. American Society for Parenteral and Enteral Nutrition.
- NANDA International. (2023). NANDA-I nursing diagnoses: Definitions & classification 2023-2025. NANDA International.
- National Institutes of Health. (2023). Guidelines for skin and wound care. National Institutes of Health.
- National Pressure Ulcer Advisory Panel. (2023). Prevention and treatment of pressure ulcers. National Pressure Ulcer Advisory Panel.
- World Health Organization. (2023). Global guidelines on pressure ulcer prevention and management. World Health Organization.