Impaired gas exchange occurs when the lungs cannot effectively exchange oxygen and carbon dioxide, leading to symptoms like shortness of breath and cyanosis. A focused nursing care plan for impaired gas exchange is vital to improve oxygenation and prevent complications.
You can
Scenario
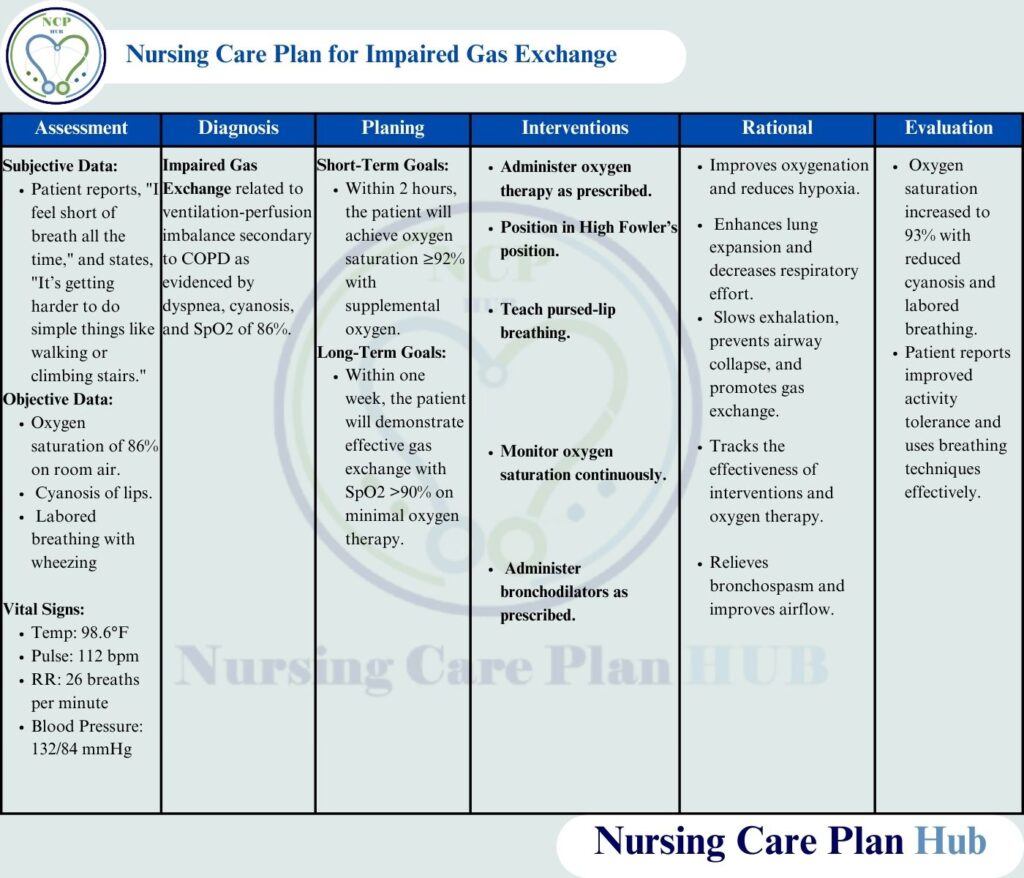
Patient Background: Sarah, a 65-year-old female with a history of chronic obstructive pulmonary disease (COPD), presents to the emergency department with complaints of shortness of breath, wheezing, and cyanosis of the lips. Her oxygen saturation is 86% on room air, and she has labored breathing. The patient reports increased fatigue over the past three days and difficulty completing daily activities. Sarah is a smoker with a 40-pack-year history.
Education for Patient
What is Impaired Gas Exchange?
The inability to adequately exchange oxygen and carbon dioxide at the alveolar-capillary level, leading to reduced oxygenation of tissues and retention of carbon dioxide (World Health Organization, 2023). This forms the basis for the nursing care plan for impaired gas exchange in conditions like COPD and pneumonia.
Pathophysiology of Impaired Gas Exchange
Impaired gas exchange occurs when alveolar ventilation is compromised due to factors like inflammation, mucus production, or alveolar damage, as seen in COPD and pneumonia impaired gas exchange. These disruptions lead to hypoxemia (low oxygen levels) and hypercapnia (high carbon dioxide levels), causing symptoms such as dyspnea and cyanosis. Conditions like asthma nursing diagnosis impaired gas exchange highlight airway constriction, further hindering effective gas exchange at the alveolar-capillary level. According to the National Institutes of Health (NIH), this results in hypoxemia and hypercapnia, causing respiratory distress (National Institutes of Health, 2023).
Common Causes of Impaired Gas Exchange
- Chronic lung diseases such as COPD, asthma, and pneumonia.
- Pulmonary embolism or blood clots in the lungs.
- Respiratory muscle weakness.
- Airway obstruction from excessive mucus or bronchospasm (e.g., impaired gas exchange related to COPD).
- Alveolar damage due to smoking or environmental toxins.
Risk Factors in COPD and Asthma
- Smoking (e.g., 40-pack-year history contributing to COPD impaired gas exchange).
- Exposure to air pollution or occupational hazards.
- Advanced age increasing susceptibility.
- Obesity affecting breathing mechanics.
- Recurrent or chronic lung infections.
Early Indicators for Nursing Diagnosis for impaired gas exchange
- Shortness of breath (dyspnea).
- Cyanosis of lips or extremities.
- Tachypnea and labored breathing.
- Fatigue and decreased activity tolerance.
- Wheezing or abnormal lung sounds, especially in impaired gas exchange nursing diagnosis related to asthma.
- Confusion or lethargy in severe cases due to hypoxia.
Complications
- Respiratory failure requiring mechanical ventilation.
- Cardiac strain or right-sided heart failure.
- Tissue hypoxia leading to organ dysfunction.
- Acute respiratory distress syndrome (ARDS) in nursing care plans for pneumonia impaired gas exchange.
- Increased risk of infections due to impaired immunity.
Importance of a Nursing Care Plan for Impaired Gas Exchange
A well-structured nursing care plan for impaired gas exchange is essential to address respiratory issues effectively. It provides a systematic approach to identifying and managing symptoms such as shortness of breath, cyanosis, and reduced oxygen saturation. This care plan ensures that interventions like oxygen therapy and breathing exercises are tailored to the patient’s condition, improving outcomes in cases like impaired gas exchange related to COPD or pneumonia. By setting clear goals and monitoring progress, the plan helps prevent complications such as respiratory failure, ensuring optimal oxygenation and patient recovery.
Also Read: Nursing Care Plan for Impaired Skin Integrity: Pressure Ulcer
Comprehensive Assessment
Assess Respiratory Status
- Rationale: Monitoring respiratory rate, rhythm, and depth helps identify the severity of the impairment (National Institutes of Health, 2023).
- How to Perform: Observe chest movement, count respiratory rate for one minute, and note accessory muscle use or nasal flaring.
Monitor Oxygen Saturation Levels
- Rationale: SpO2 levels provide insight into the patient’s oxygenation status and the effectiveness of oxygen therapy (American Lung Association, 2023).
- How to Perform: Use a pulse oximeter to measure oxygen saturation continuously or at regular intervals.
Auscultate Lung Sounds
- Rationale: Wheezing, crackles, or diminished breath sounds may indicate airway obstruction or fluid accumulation (World Health Organization, 2023).
- How to Perform: Use a stethoscope to listen to all lung fields, comparing bilaterally for abnormal sounds.
Assess for Signs of Hypoxia
- Rationale: Cyanosis, confusion, and restlessness are clinical indicators of inadequate oxygen delivery to tissues (American Lung Association, 2023).
- How to Perform: Inspect skin and mucous membranes for cyanosis and evaluate mental status for confusion or agitation.
Evaluate Arterial Blood Gases (ABGs)
- Rationale: ABG analysis provides detailed information on oxygenation, ventilation, and acid-base balance (National Institutes of Health, 2023).
- How to Perform: Assist in drawing ABG samples and interpret results for PaO2, PaCO2, and pH values.
Assess for Contributing Factors
- Rationale: Identifying underlying conditions such as infection or airway obstruction guides targeted treatment (World Health Organization, 2023).
- How to Perform: Obtain a detailed patient history and perform a physical examination focusing on symptoms such as fever or productive cough.
Nursing Diagnoses
- Impaired Gas Exchange related to ventilation-perfusion imbalance secondary to COPD as evidenced by oxygen saturation of 86%, dyspnea, and cyanosis (NANDA International, 2023).
- Ineffective Airway Clearance related to excessive mucus production and bronchospasm as evidenced by wheezing and labored breathing (NANDA International, 2023).
SMART Goals for Impaired Gas Exchange
- Short-Term Goal: Within 2 hours, Sarah will achieve improved oxygen saturation levels of ≥92% with supplemental oxygen and show reduced signs of respiratory distress (American Lung Association, 2023).
- Long-Term Goal: Within one week, Sarah will demonstrate effective gas exchange with improved activity tolerance, maintaining SpO2 >90% on minimal oxygen therapy (National Institutes of Health, 2023).
Nursing Interventions with Rationale
Administer Supplemental Oxygen as Prescribed
- Rationale: Oxygen therapy improves oxygenation and reduces hypoxia (American Lung Association, 2023).
- How to Perform: Use a nasal cannula or mask to deliver the prescribed oxygen concentration. Monitor for signs of oxygen toxicity in long-term therapy.
Position the Patient in High Fowler’s Position
- Rationale: Sitting upright facilitates lung expansion, reducing dyspnea and improving ventilation (National Institutes of Health, 2023).
- How to Perform: Assist Sarah into a sitting position with the head of the bed elevated to at least 45–90 degrees.
Encourage Pursed-Lip Breathing
- Rationale: This technique slows exhalation, preventing airway collapse and promoting gas exchange (American Lung Association, 2023).
- How to Perform: Teach Sarah to inhale through her nose and exhale slowly through pursed lips, as though blowing out a candle.
Perform Chest Physiotherapy
- Rationale: Percussion and vibration techniques help loosen mucus in the lungs, facilitating clearance (World Health Organization, 2023).
- How to Perform: Use cupped hands to percuss Sarah’s back and chest, focusing on lung segments with decreased breath sounds.
Administer Bronchodilators and Mucolytics as Prescribed
- Rationale: These medications reduce bronchospasm and thin mucus, improving airflow and gas exchange (National Institutes of Health, 2023).
- How to Perform: Administer medications via nebulizer or inhaler, ensuring Sarah understands proper usage techniques.
Promote Adequate Hydration
- Rationale: Hydration helps thin secretions, making them easier to clear from the airways (American Lung Association, 2023).
- How to Perform: Encourage fluid intake of at least 2 liters per day, unless contraindicated by other conditions.
Monitor ABG and Electrolyte Levels
- Rationale: Regular monitoring identifies hypoxemia, hypercapnia, and imbalances that may require intervention (National Institutes of Health, 2023).
- How to Perform: Collect blood samples as ordered and compare results to baseline values.
Evaluation
- Oxygen saturation increased to 93% with reduced cyanosis and labored breathing.
- Patient reports improved activity tolerance and uses breathing techniques effectively.
- Improved Oxygenation: Sarah’s oxygen saturation improved to 94% with oxygen therapy, and she exhibits reduced cyanosis and dyspnea.
- Effective Breathing: Sarah demonstrates the ability to use pursed-lip breathing effectively and reports decreased respiratory effort.
- Clear Airway: Lung sounds improved with reduced wheezing, and Sarah successfully expectorates mucus.
- Knowledge Retention: Sarah verbalizes understanding of breathing techniques, medication use, and smoking cessation benefits.
Here you can download the pdf file of ncp on Impaired Gas Exchange by clicking on download button below:
References
- American Lung Association. (2023). Chronic obstructive pulmonary disease management.
- NANDA International. (2023). NANDA-I nursing diagnoses: Definitions & classification 2023-2025.
- National Institutes of Health. (2023). Respiratory disorders and gas exchange guidelines.
- World Health Organization. (2023). Global respiratory care strategies and interventions.

Keep up the good work