Gastroenteritis, a common condition characterized by inflammation of the stomach and intestines, requires a thorough nursing care plan for gastroenteritis to address its symptoms and prevent complications. Whether in pediatric or adult cases, creating a comprehensive acute gastroenteritis nursing care plan is crucial for effective management.
You can
Scenario
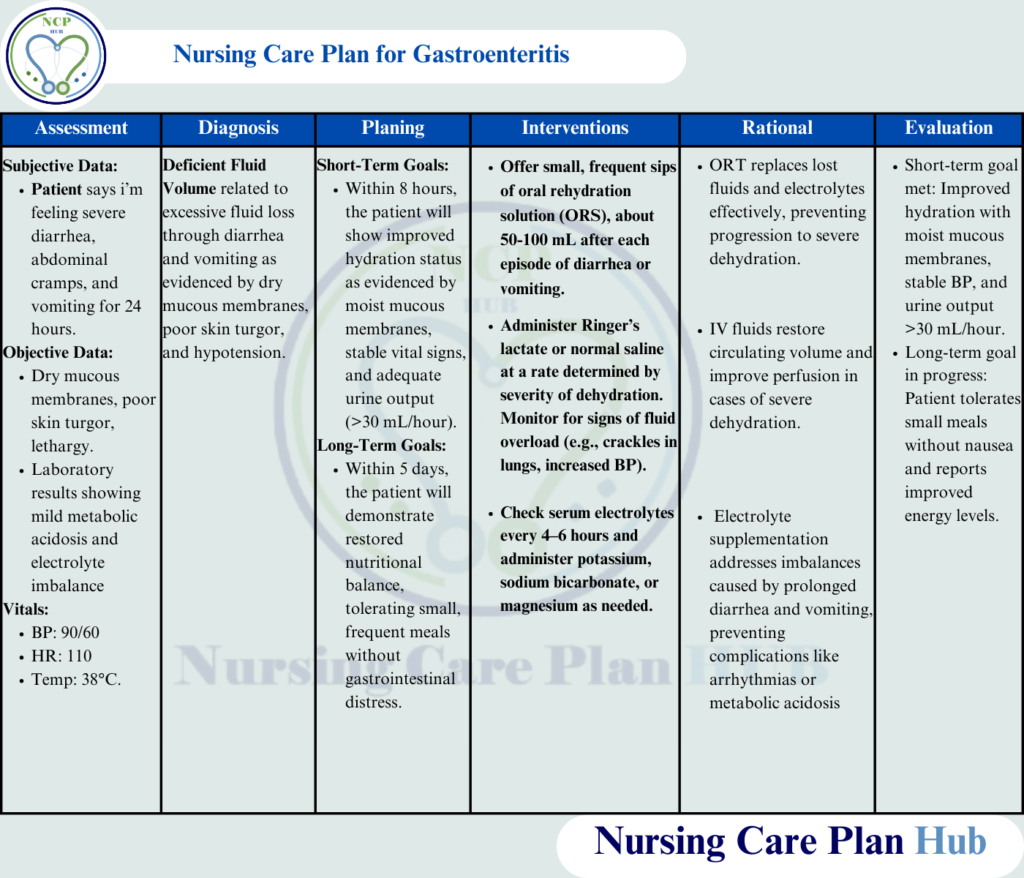
Patient Background: Ahsan, a 24-year-old male, presents to the emergency department with complaints of severe diarrhea, abdominal cramps, and vomiting for the past 24 hours. He reports having eaten at a roadside stall two days ago. On examination, he appears lethargic, with dry mucous membranes and poor skin turgor. His vital signs show a blood pressure of 90/60 mmHg, heart rate of 110 bpm, and temperature of 38°C. Laboratory results indicate mild metabolic acidosis and electrolyte imbalance.
Education for Patient
What Is Gastroenteritis?
Gastroenteritis is a medical condition characterized by inflammation of the stomach and intestines. It commonly results from infections caused by viruses, bacteria, or parasites. The condition is marked by symptoms such as diarrhea, vomiting, abdominal pain, and cramping. According to the World Health Organization (2023), gastroenteritis is a leading cause of dehydration and malnutrition, particularly in children and older adults. Early implementation of a care plan for gastroenteritis can minimize risks.
Pathophysiology Behind Acute Gastroenteritis
The gastrointestinal tract normally absorbs nutrients and water while maintaining a delicate balance between secretion and absorption. In gastroenteritis, infectious pathogens like viruses (e.g., rotavirus, norovirus), bacteria (e.g., E. coli, Salmonella), or parasites (e.g., Giardia) invade or release toxins in the intestines. These pathogens interfere with normal digestion by:
- Damaging the intestinal lining.
- Triggering inflammatory responses.
- Disrupting water and electrolyte absorption.
This results in excessive fluid secretion into the intestines, leading to diarrhea, dehydration, and electrolyte imbalances.
Causes
Gastroenteritis is primarily caused by consuming contaminated food or water. Additional causes include:
- Viral infections: Rotavirus and norovirus are the most common culprits.
- Bacterial infections: Such as Salmonella, Shigella, Campylobacter, and E. coli.
- Parasitic infections: Including Giardia lamblia and Entamoeba histolytica.
- Poor hygiene practices: Such as not washing hands after using the restroom or before meals.
- Person-to-person transmission: Common in crowded or unsanitary conditions.
Risk Factors
Certain factors can increase the likelihood of developing gastroenteritis:
- Consuming unsafe food or beverages: Raw or undercooked foods, unpasteurized dairy, or untreated water.
- Poor sanitation: Inadequate sewage disposal and lack of clean water.
- Traveling to endemic regions: Developing countries often report higher rates of waterborne and foodborne gastroenteritis.
- Weakened immune system: Individuals with chronic illnesses or on immunosuppressive therapy are more vulnerable.
- Age: Infants, young children, and elderly individuals are at higher risk due to their weaker immunity.
Such risks make tailored ncp for gastroenteritis critical, especially in infants or immunocompromised individuals.
Symptoms
The clinical manifestations of gastroenteritis can vary but typically include:
- Diarrhea: Ranging from mild to severe, often watery and sometimes with blood (dysentery).
- Vomiting and nausea: Leading to fluid loss and reduced appetite.
- Abdominal cramps: Intermittent and sharp pain in the stomach region.
- Fever: Often mild but can be severe in bacterial infections.
- Dehydration: Symptoms include dry mouth, decreased urination, sunken eyes, and lethargy.
- Fatigue: Resulting from electrolyte imbalance and lack of nutrients.
These symptoms guide the development of a nursing care plan for diarrhea and vomiting or a nursing care plan for diarrhea related to gastroenteritis.
Complications
If left untreated, gastroenteritis can lead to severe health complications:
- Severe dehydration: Rapid fluid loss can result in life-threatening dehydration, particularly in children and the elderly.
- Electrolyte imbalance: Loss of sodium, potassium, and other electrolytes can disrupt heart and muscle function.
- Kidney dysfunction: Prolonged dehydration can impair kidney function, leading to acute kidney injury.
- Shock: Severe cases may progress to hypovolemic shock, a critical condition caused by reduced blood volume.
Prevention of these outcomes is central to the plan of care for a client who has gastroenteritis.
Key Points for Patient Awareness
- Hydration is critical: Drink plenty of fluids, such as oral rehydration solutions (ORS), to replace lost electrolytes.
- Hygiene matters: Practice proper handwashing, especially before eating and after using the restroom.
- Food safety: Avoid raw or undercooked foods and ensure water is boiled or treated in areas with poor sanitation.
- Seek medical attention: If symptoms persist or worsen, such as signs of dehydration or high fever, consult a healthcare provider promptly.
Also Read: Nursing Care Plan on Insomnia
Assessment in a Nursing Care Plan for Gastroenteritis
Assess Hydration Status
- Rationale: Dehydration is a major complication often addressed in a nursing care plan for gastroenteritis, requiring prompt identification (World Health Organization, 2023).
- How to Perform: Monitor skin turgor, mucous membranes, and urine output. Look for signs of severe dehydration such as sunken eyes and a dry tongue.
Monitor Vital Signs
- Rationale: Hypotension, tachycardia, and fever are critical indicators of fluid loss and systemic response to infection, essential in managing a nursing care plan for gastroenteritis (National Institutes of Health, 2023).
- How to Perform: Measure blood pressure, heart rate, respiratory rate, and temperature every 2-4 hours.
Evaluate Gastrointestinal Symptoms
- Rationale: The frequency, volume, and characteristics of diarrhea and vomiting help determine the severity and progression, key components of a comprehensive nursing care plan for gastroenteritis (Centers for Disease Control and Prevention, 2023).
- How to Perform: Ask the patient to describe stool characteristics (e.g., watery, bloody) and vomiting episodes.
Assess for Electrolyte Imbalance
- Rationale: Loss of electrolytes like sodium, potassium, and bicarbonate can cause complications like arrhythmias or metabolic acidosis, often detailed in nursing care plans for gastroenteritis (National Institutes of Health, 2023).
- How to Perform: Monitor lab results, including serum electrolytes and arterial blood gases.
Monitor Intake and Output
- Rationale: Measuring fluid intake and output provides a clear picture of hydration status and guides fluid replacement, vital in the nursing care plan for gastroenteritis (World Health Organization, 2023).
- How to Perform: Record oral and intravenous fluid intake and monitor urine output using a calibrated container.
Check for Signs of Shock
- Rationale: Severe dehydration, a common complication in gastroenteritis, can lead to hypovolemic shock, which is life-threatening if untreated. This step is essential in a nursing care plan for gastroenteritis (Centers for Disease Control and Prevention, 2023).
- How to Perform: Observe for cold, clammy skin, weak pulse, or confusion..
NANDA Nursing Diagnosis for Acute Gastroenteritis
- Deficient Fluid Volume related to excessive fluid loss through diarrhea and vomiting as evidenced by dry mucous membranes, poor skin turgor, and hypotension (NANDA International, 2023).
- Imbalanced Nutrition: Less than Body Requirements related to decreased intake and absorption as evidenced by lethargy and weight loss (NANDA International, 2023).
Goals in Nursing Care Plan for Gastroenteritis
Short-Term Goal in Nursing Care Plan for Gastroenteritis:
Within 8 hours, Ahsan will show improved hydration status as evidenced by moist mucous membranes, stable vital signs, and adequate urine output (>30 mL/hour).
Long-Term Goal in Nursing Care Plan for Gastroenteritis:
Within 5 days, Ahsan will demonstrate restored nutritional balance, tolerating small, frequent meals without gastrointestinal distress.
Interventions in Nursing Care Plan for Gastroenteritis
Administer Oral Rehydration Therapy (ORT)
- Rationale: ORT is essential in the nursing care plan for diarrhea related to gastroenteritis. It effectively replaces lost fluids and electrolytes, particularly in mild to moderate dehydration (World Health Organization, 2023).
- How to Perform: Offer small, frequent sips of ORS solution. Encourage drinking after each episode of diarrhea or vomiting.
Initiate Intravenous Fluid Therapy as Prescribed
- Rationale: IV fluids restore intravascular volume quickly in cases of severe dehydration, a critical aspect of the nursing care plan for acute gastroenteritis (National Institutes of Health, 2023).
- How to Perform: Administer Ringer’s lactate or normal saline as ordered, monitoring for signs of fluid overload.
Monitor Electrolyte Levels and Administer Supplements
- Rationale: Electrolyte supplementation addresses deficiencies caused by diarrhea and vomiting, a common issue in gastroenteritis nursing diagnoses (Centers for Disease Control and Prevention, 2023).
- How to Perform: Administer potassium or sodium bicarbonate as prescribed, guided by lab results.
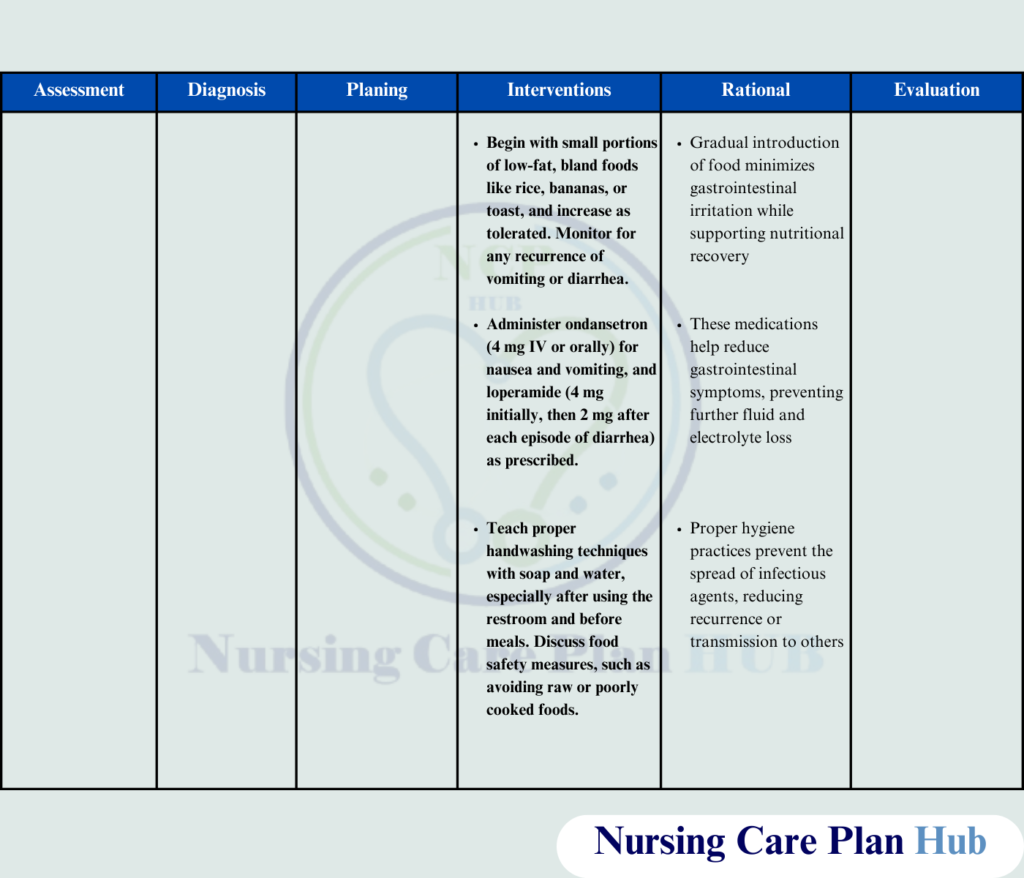
Encourage Gradual Oral Intake of Easily Digestible Foods
- Rationale: Starting with bland, low-fat foods supports gastrointestinal recovery and aligns with the nursing care plan for gastroenteritis in infants and adults (World Health Organization, 2023).
- How to Perform: Begin with foods like rice, bananas, or toast and advance the diet as tolerated.
Administer Antiemetic and Antidiarrheal Medications as Prescribed
- Rationale: These medications reduce symptoms and prevent further fluid loss, crucial in the plan of care for a client who has gastroenteritis (National Institutes of Health, 2023).
- How to Perform: Administer medications such as ondansetron for vomiting or loperamide for diarrhea, ensuring proper dosing.
Educate on Hygiene Practices
- Rationale: Proper handwashing and food safety practices prevent the spread and recurrence of gastroenteritis, key components of any ncp for gastroenteritis (Centers for Disease Control and Prevention, 2023).
- How to Perform: Teach the patient about proper handwashing, safe food preparation, and avoiding street food.
Monitor for Signs of Improvement or Deterioration
- Rationale: Early detection of worsening symptoms ensures timely intervention, aligning with nursing intervention for gastroenteritis (World Health Organization, 2023).
- How to Perform: Regularly reassess hydration, electrolyte balance, and gastrointestinal symptoms.
Evaluation of a Nursing Care Plan for Acute Gastroenteritis
- Improved Hydration: Ahsan’s mucous membranes are moist, skin turgor is normal, and urine output exceeds 30 mL/hour.
- Nutritional Recovery: Ahsan tolerates small, frequent meals without nausea or abdominal pain.
- Knowledge Retention: Ahsan verbalizes understanding of hygiene practices and dietary modifications to prevent recurrence.
Here you can download the PDF file of nursing care plan for Gastroenteritis
References
- Centers for Disease Control and Prevention. (2023). Gastrointestinal infections and management.
- NANDA International. (2023). NANDA-I nursing diagnoses: Definitions & classification 2023-2025.
- National Institutes of Health. (2023). Gastroenteritis: Causes, symptoms, and treatment options.
- World Health Organization. (2023). Management of acute diarrhea and dehydration.cam
Top of Form
Bottom of Form

i like this