Fluid volume deficit is a common issue in pediatric patients, especially during heat-related conditions like heat stroke. Below is a comprehensive care plan for fluid volume deficit, focusing on Ahmed, a 7-year-old boy experiencing dehydration symptoms.
You can Downlaod the nursing care plan for fluid volume deficit in
Scenario
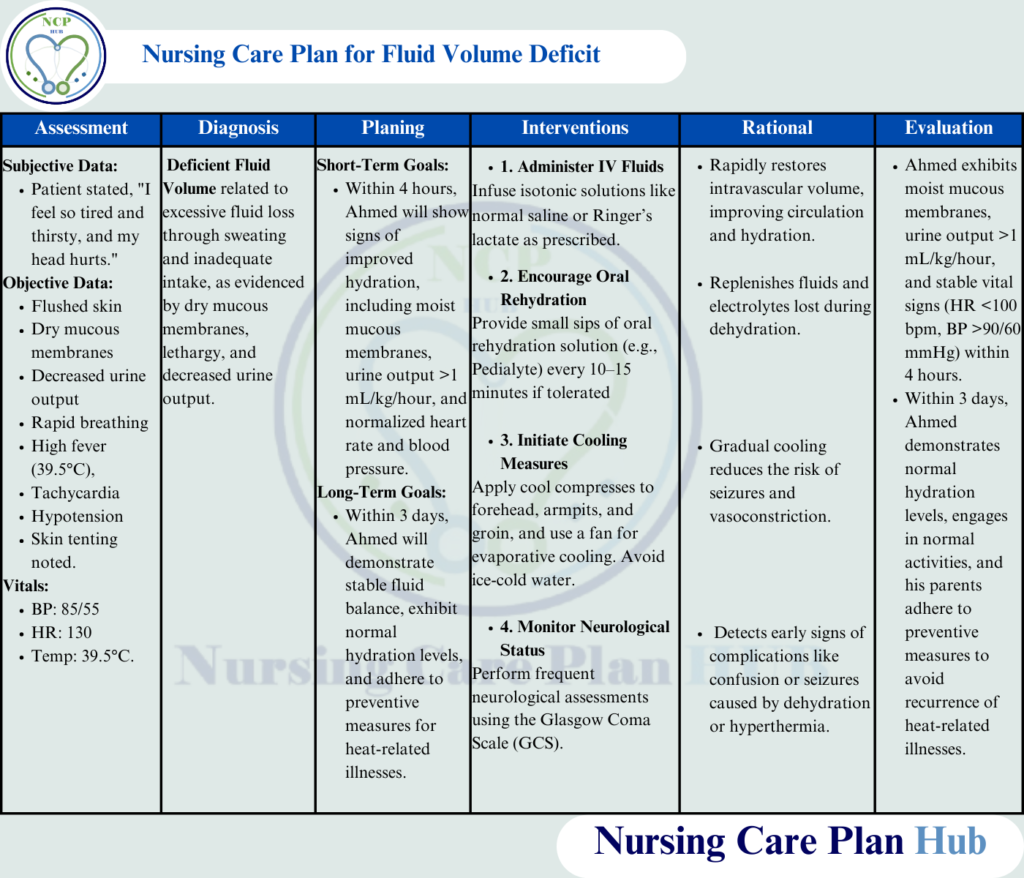
Patient Background: Ahmed, a 7-year-old boy, is brought to the emergency department by his parents after playing outdoors in extreme heat for several hours. His symptoms include lethargy, flushed skin, dry mucous membranes, decreased urine output, and rapid breathing. Vital signs reveal a high fever of 39.5°C, tachycardia (HR: 130 bpm), and hypotension (BP: 85/55 mmHg). Ahmed appears irritable and fatigued, with skin tenting noted during physical examination. Laboratory results indicate increased hematocrit levels, elevated serum sodium, and mild metabolic acidosis. The folowing nursing care plan for fluid volume deficit will help to manage patiens with scenario like this.
Education for Patient and Family
Providing education is essential to prevent recurrence of dehydration and ensure effective management of fluid volume deficit. An Effective Care Plan for Fluid Volume Deficit will meet this goal.
What is Fluid Volume Deficit?
According to the World Health Organization (WHO), fluid volume deficit, or dehydration, is a condition that occurs when the body loses more water and essential electrolytes than it takes in, impairing normal body functions (World Health Organization, 2023).
Pathophysiology of Fluid Volume Deficit
The National Institutes of Health (NIH) explains that fluid volume deficit results from excessive fluid loss, inadequate fluid intake, or a combination of both. In dehydration, there is a reduction in extracellular fluid volume, leading to decreased organ perfusion and metabolic imbalances. In severe cases, hypovolemia may occur, impacting cardiovascular and renal functions (National Institutes of Health, 2023).
Causes and Risk Factors
- Highlight that playing outdoors in extreme heat without adequate hydration is a significant risk factor for developing fluid volume deficit nursing diagnosis.
- Discuss other triggers like vomiting, diarrhea, or high fever, which may lead to the need for a nursing care plan for dehydration related to vomiting.
Preventive Measures
- Encourage regular water intake during physical activities or hot weather to avoid conditions requiring a care plan for fluid volume deficit.
- Recommend giving children oral rehydration solutions (ORS) during illnesses to balance fluids and electrolytes.
Signs to Watch For
- Teach parents to recognize early symptoms like dry mouth, lethargy, and reduced urine output, which are indicators of the need for a fluid volume deficit nursing care plan.
- Emphasize the importance of observing physical signs such as skin tenting or irritability.
When to Seek Medical Attention
- Stress the importance of seeking medical care if severe symptoms like fainting, confusion, or inability to drink fluids occur.
- Explain how prompt action can prevent complications requiring intensive nursing interventions for fluid volume deficit.
Long-Term Hydration Strategies
- Advise families on maintaining consistent hydration habits at home to avoid conditions necessitating nursing care for dehydration.
- Emphasize that proper hydration prevents the recurrence of dehydration nursing diagnoses and promotes overall health.
Also Read: Nursing Care Plan for Gastroenteritis
Comprehensive Assessment for Fluid Volume Deficit in Pediatric Patients
Assess Hydration Status
- What to Check: Skin turgor, mucous membranes, capillary refill time, and thirst level to identify signs of fluid volume deficit.
- Rationale: Fluid loss affects tissue hydration, and early identification can prevent complications like hypovolemic shock caused by dehydration.
- How to Perform: Pinch the skin on the abdomen or forearm; if the skin remains tented, it indicates dehydration. Observe mucous membranes for dryness, a common indicator of fluid volume deficit nursing diagnosis.
Monitor Vital Signs
- What to Monitor: Blood pressure, heart rate, temperature, and respiratory rate to assess the severity of the patient’s dehydration nursing diagnosis.
- Rationale: Vital signs provide critical information about circulatory and respiratory status, which are often affected in cases of fluid volume deficit.
- How to Perform: Use pediatric-sized equipment to measure vitals every 15–30 minutes until stable, ensuring the nursing care plan for dehydration aligns with the patient’s needs.
Evaluate Neurological Status
- What to Observe: Level of consciousness, irritability, and lethargy as part of the nursing care for dehydration.
- Rationale: Dehydration and heat stroke can cause neurological impairments, contributing to the nursing diagnosis of fluid volume deficit.
- How to Perform: Use the Glasgow Coma Scale (GCS) to evaluate responsiveness and cognitive function.
Monitor Fluid Intake and Output
- What to Measure: Oral and intravenous fluid intake, urine output, and stool consistency (if diarrhea is present) to assess fluid volume deficit nursing care plan effectiveness.
- Rationale: Accurate measurement ensures fluid replacement aligns with deficits and addresses dehydration nursing diagnosis effectively.
- How to Perform: Use a pediatric urine bag or catheter to collect urine. Document intake/output hourly to track progress in the nursing care plan for dehydration related to vomiting or other causes.
Assess for Electrolyte Imbalance
- What to Look For: Muscle weakness, fatigue, irregular heart rhythms, and lab values for sodium, potassium, and chloride, common in dehydration nursing diagnosis cases.
- Rationale: Electrolyte imbalances are common in dehydration and fluid volume deficit. Monitoring them ensures effective nursing intervention for fluid volume deficit.
- How to Perform: Monitor laboratory results and observe for physical signs like muscle cramps or arrhythmias, adjusting interventions as necessary.
Examine Skin for Heat Damage
- What to Observe: Skin color, texture, and signs of erythema or dryness to assess the severity of fluid volume deficit caused by heat exposure.
- Rationale: Skin changes are common indicators of dehydration severity and guide the fluid volume deficit nursing care plan.
- How to Perform: Palpate for warmth, inspect for redness or burns, and check for the presence or absence of sweat.
Observe for Circulatory Compromise
- What to Assess: Peripheral pulses, capillary refill, and skin temperature to monitor for signs of hypovolemia in fluid volume deficit nursing diagnosis.
- Rationale: Dehydration can lead to reduced perfusion and circulatory failure, which must be addressed in the nursing care plan on dehydration.
- How to Perform: Check radial or brachial pulses and observe for pallor or cyanosis as part of continuous assessment.
Nursing Diagnoses
- Deficient Fluid Volume related to excessive fluid loss through sweating and inadequate intake, as evidenced by dry mucous membranes, lethargy, and decreased urine output (NANDA International, 2023).
- Hyperthermia related to prolonged exposure to high environmental temperature, as evidenced by flushed skin, high fever, and irritability (NANDA International, 2023).
Goals of the Nursing Care Plan for Fluid Volume Deficit
- Short-Term Goal: Within 4 hours, Ahmed will show signs of improved hydration, including moist mucous membranes, urine output >1 mL/kg/hour, and normalized heart rate and blood pressure.
- Long-Term Goal: Within 3 days, Ahmed will demonstrate stable fluid balance, exhibit normal hydration levels, and adhere to preventive measures for heat-related illnesses.
Nursing Interventions for Fluid Volume Deficit and Dehydration
Administer Intravenous Fluids as Prescribed
- Rationale: IV fluids restore intravascular volume quickly, correcting fluid volume deficit and addressing dehydration nursing diagnosis, including electrolyte imbalances.
- How to Perform: Infuse isotonic solutions like normal saline or Ringer’s lactate at a rate appropriate for the child’s weight and condition. Monitor for signs of fluid overload, such as edema or crackles in the lungs, as part of the fluid volume deficit nursing care plan.
Encourage Oral Rehydration Therapy (ORT)
- Rationale: ORT prevents further dehydration and replenishes electrolytes in mild to moderate cases.
- How to Perform: Offer small sips of oral rehydration solutions (e.g., Pedialyte) every 10–15 minutes to ensure alignment with the nursing care plan on dehydration.
Initiate Cooling Measures
- Rationale: Lowering core body temperature reduces the risk of seizures and organ damage associated with severe dehydration and fluid volume deficit.
- How to Perform: Apply cool compresses to the forehead, armpits, and groin. Use fans or tepid sponging for cooling while avoiding ice-cold water to prevent vasoconstriction. This intervention is critical for patients with dehydration nursing diagnosis and heat-related complications.
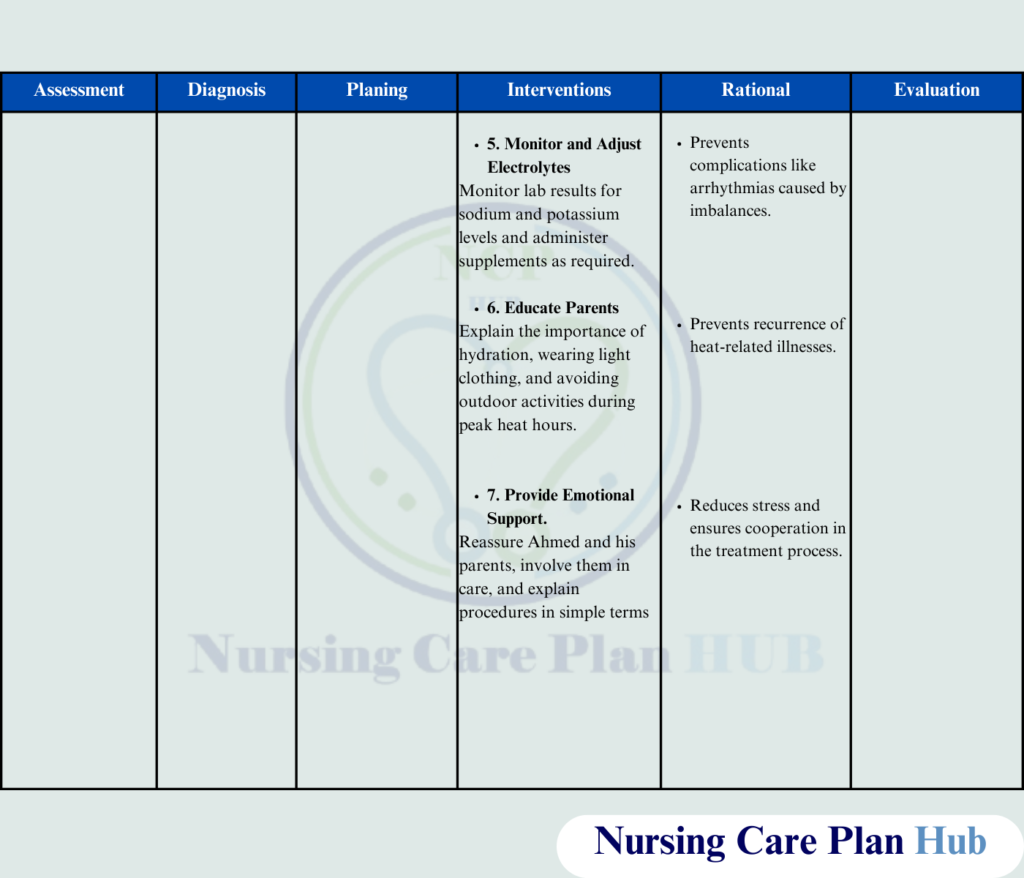
Monitor and Correct Electrolyte Imbalances
- Rationale: Electrolytes like sodium and potassium are vital for cardiac and neurological functions, making this step crucial in managing nursing intervention for fluid volume deficit.
- How to Perform: Administer supplements or adjust fluids based on lab results. Monitor for side effects like hyperkalemia or hypokalemia, ensuring adherence to the fluid volume deficit nursing care plan.
Educate Parents About Prevention
- Rationale: Knowledge of dehydration and fluid volume deficit risk factors helps prevent recurrence and supports the effectiveness of the nursing care plan for dehydration related to vomiting or heat exposure.
- How to Perform: Explain the importance of adequate hydration, wearing light clothing, and avoiding outdoor activity during peak heat hours as part of the overall nursing care for dehydration strategy.
Assess Skin and Mucous Membranes Regularly
- Rationale: Early detection of dehydration signs like dry mucous membranes or poor skin turgor prevents worsening fluid volume deficit nursing diagnosis.
- How to Perform: Inspect mucous membranes for dryness and skin for turgor every 2 hours, adjusting the nursing care plan on dehydration as needed.
Provide Emotional Support to the Child and Family
- Rationale: Hospitalization can be stressful for children and parents, impacting their overall experience during treatment for fluid volume deficit.
- How to Perform: Offer reassurance, involve parents in care, and provide age-appropriate explanations to the child, promoting adherence to the care plan for fluid volume deficit.
Evaluation
- Hydration Improvement: Ahmed exhibits moist mucous membranes, normal skin turgor, and urine output >1 mL/kg/hour.
- Temperature Regulation: Ahmed’s body temperature is within the normal range (<37.5°C) without signs of irritability or confusion.
- Parental Understanding: Ahmed’s parents demonstrate understanding of heat stroke prevention measures and commit to ensuring adequate hydration and heat protection.
Here you can download the PDF file of nursing care plan for fluid volume deficit.
References
- Centers for Disease Control and Prevention. (2023). Heat-related illnesses: Prevention and management.
- NANDA International. (2023). NANDA-I nursing diagnoses: Definitions & classification 2023-2025.
- National Institutes of Health. (2023). Pediatric dehydration and heat illnesses.
- World Health Organization. (2023). Management of dehydration and heat-related illnesses in children.
