When we talk about patient care, one of the most valuable tools used by doctors and nurses is the patient case file. A case file like Liver Cirrhosis Management is more than just paperwork—it’s a detailed record that captures everything about a person’s health journey. From their medical history and current complaints to test results and treatment progress, it tells the story of the illness and guides decisions about care.
For healthcare professionals, these files aren’t just about documentation. They are the backbone of safe and effective care. Nurses rely on them to identify needs, track changes, and create individualized care plans. Doctors use them to decide on the right interventions and adjust treatments. Students and researchers, meanwhile, turn to case files to learn from real-world scenarios, applying classroom knowledge to practical examples.
In today’s post, we’ll be diving into a case centered around liver cirrhosis management. This condition develops when healthy liver tissue is replaced with scar tissue, disrupting the organ’s vital functions. We’ll explore how cirrhosis shows up in patients, including common signs and symptoms of cirrhosis such as jaundice, swelling, and fatigue. We’ll also touch on the main causes, including hepatitis infection and long-term alcohol use, and review potential cirrhosis complications like ascites, portal hypertension, and encephalopathy.
Finally, we’ll walk through possible nursing diagnoses and care priorities for patients with this condition. By the end, you’ll see how a structured case file not only supports clinical practice but also deepens our understanding of complex diseases.
Patient Presenting complaints
Mr. K. is a 58-year-old male, a retired factory worker who lives with his spouse. His lifestyle has been largely sedentary, shaped by chronic fatigue and reduced physical activity in recent years. Before retirement, he spent decades in physically demanding work, but his habits—particularly heavy alcohol use for over 20 years—contributed significantly to his current health status.
The main reason he sought hospital care was progressive abdominal swelling, increasing breathlessness, and worsening fatigue. These concerns became particularly noticeable over the past two weeks, along with yellow discoloration of the eyes, swelling of his legs, and loss of appetite. His early satiety and reduced energy limited his ability to manage daily tasks, prompting admission for further evaluation.
Looking into his medical history, Mr. K. had been diagnosed with hepatitis C a decade ago but did not maintain regular follow-up or treatment. He also carries a history of hypertension, for which he takes medication. His family history is largely unremarkable for liver disease, although his father had type 2 diabetes. Socially, he is an ex-smoker, with alcohol cessation only three months prior to this admission. These details highlight both modifiable and long-standing risk factors contributing to his disease.
On initial presentation, Mr. K. appeared weak, cachectic, and jaundiced. He described difficulty breathing due to abdominal distension, consistent with ascites. The swelling in his legs and confusion episodes further indicated advancing complications. Together, his story paints a clear picture of decompensated cirrhosis, where the liver is no longer able to perform its normal functions, and complications such as ascites, jaundice, and early hepatic encephalopathy begin to dominate the clinical picture.
What is Liver Cirrhosis?
Liver cirrhosis is a long-term condition in which the healthy tissue of the liver is slowly replaced by scar tissue. You can imagine the liver as a sponge that filters toxins, processes nutrients, and produces vital proteins. Over time, repeated damage—whether from infections, alcohol, or other causes—creates scars, making the sponge stiff and less effective. When this scarring becomes severe, the liver cannot keep up with its many jobs, leading to serious health problems.
Pathophysiology: what happens inside the body
Pathophysiology, or “what happens inside the body,” helps explain this process. The liver normally receives blood through a large vessel called the portal vein. With cirrhosis, the scar tissue disrupts blood flow, creating a backup called portal hypertension. This increased pressure pushes fluid into the abdomen, causing ascites (fluid buildup) and makes veins in the esophagus swell, leading to esophageal varices, which can bleed dangerously. At the same time, the damaged liver produces less albumin (a protein that maintains fluid balance), worsening swelling and low blood pressure. The inability to clear toxins results in brain-related changes, known as hepatic encephalopathy, which can cause confusion and even coma.
Several risk factors make someone more vulnerable to cirrhosis. Chronic hepatitis C infection, as seen in Mr. K.’s case, is one of the leading causes worldwide. Long-term heavy alcohol consumption also plays a major role, especially when drinking habits continue over decades. Other risks include obesity (which can lead to fatty liver disease), poorly controlled diabetes, and long-term exposure to toxins or certain medications. Genetics may also increase susceptibility in some individuals.
For many patients, the early stages of cirrhosis are silent—much like rust forming inside a pipe before water flow is affected. By the time symptoms such as jaundice, fatigue, or abdominal swelling appear, significant damage has already occurred. That is why cirrhosis is often diagnosed in its advanced stages.
Understanding cirrhosis is crucial not just for healthcare workers but also for families and patients themselves. Knowing how scarring affects the liver helps explain why management is so complex. Treatments often focus on slowing progression, relieving symptoms, and preventing complications like coagulopathy, bleeding varices, or kidney strain. While the damage can’t be reversed, careful monitoring, lifestyle changes, and specific interventions (such as paracentesis for fluid removal) can greatly improve quality of life.
Signs and Symptoms of Liver Cirrhosis
When it comes to cirrhosis, the way it shows up in patients can vary depending on whether the disease is in its early or advanced stages. In Mr. K.’s case, many of the features point toward decompensated cirrhosis, where the liver has already lost much of its reserve.
Subjective Data (Patient-Reported)
- Fatigue and weakness – a common early symptom due to the liver’s reduced ability to process nutrients.
- Loss of appetite and early satiety – feeling full quickly because of abdominal fluid buildup (ascites).
- Abdominal distension – discomfort and shortness of breath from pressure inside the belly.
- Yellowing of the eyes (jaundice) – noticed by the patient and family.
- Confusion and forgetfulness – early signs of hepatic encephalopathy, often described as “mental fog.”
Objective Data (Clinical Findings)
- Jaundice visible on skin and sclera.
- Ascites detected by a distended abdomen and shifting dullness on exam.
- Hepatomegaly (enlarged liver) palpable under the rib cage.
- Pedal edema (swelling of legs), worsened by low albumin levels.
- Spider angiomas and palmar erythema – skin changes linked with liver dysfunction.
- Labored breathing due to ascites pressing on the diaphragm.
- Neurological changes like disorientation, pointing to advanced encephalopathy.
- Lab results: low platelets, prolonged INR, and high bilirubin reflecting poor liver function and coagulopathy.
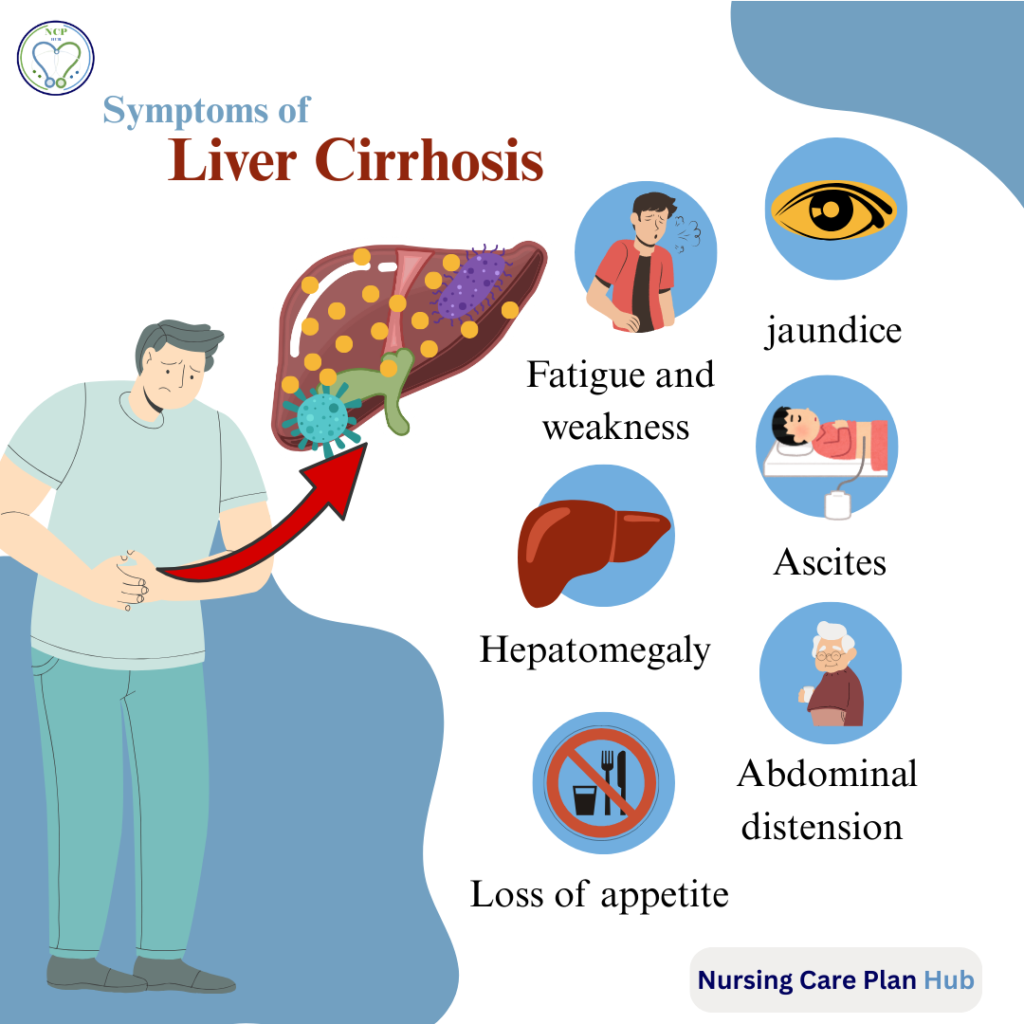
By dividing patient-reported experiences from observable signs, healthcare teams get a clearer picture of how cirrhosis is progressing, which helps guide liver cirrhosis management and treatment planning.
Causes of Liver Cirrhosis
Liver cirrhosis doesn’t develop overnight—it’s usually the result of years of repeated liver injury. The most common causes include:
- Chronic viral infections such as hepatitis B and C, which inflame and damage liver cells.
- Alcohol abuse, where long-term heavy drinking overwhelms the liver’s ability to repair itself.
- Nonalcoholic fatty liver disease (NAFLD), often linked with obesity and diabetes.
- Autoimmune hepatitis and genetic disorders (e.g., hemochromatosis, Wilson’s disease).
- Long-term toxin or medication exposure, which gradually scars the liver.
When considering risk factors, it helps to separate what can be changed (modifiable) from what cannot (non-modifiable).
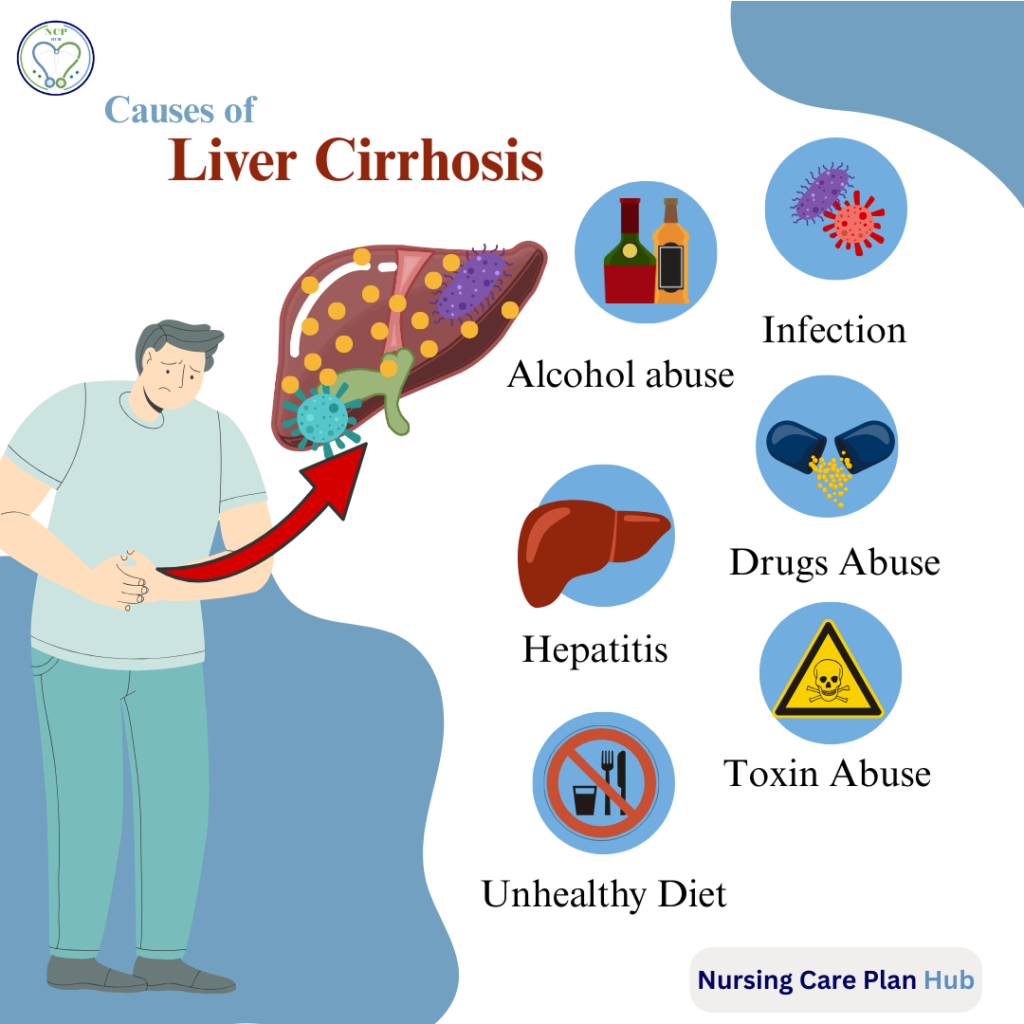
Modifiable risk factors:
- Heavy alcohol use – in Mr. K.’s case, daily drinking for over 20 years.
- Poor follow-up for chronic hepatitis C infection.
- Sedentary lifestyle and poor diet, both of which worsen liver strain.
Non-modifiable risk factors:
- Age – cirrhosis is more likely in older adults.
- Male gender, which has been linked to higher risk of alcohol-related cirrhosis.
- Genetic predispositions (though not evident in Mr. K.’s history).
For Mr. K., the combination of alcohol dependence and hepatitis C created a double hit to his liver. His age and limited physical activity added further strain. Recognizing these risk factors is crucial because targeting the modifiable ones—like abstaining from alcohol or treating viral hepatitis—can slow or prevent progression in other patients at risk.
Complications of Liver Cirrhosis
Cirrhosis is often described as a “silent” disease until complications appear. Once they do, they significantly change a patient’s quality of life and care needs.
Short-Term Complications
- Ascites: Fluid buildup in the abdomen leads to discomfort, difficulty breathing, and frequent hospital visits for paracentesis (fluid removal).
- Variceal bleeding: Enlarged veins in the esophagus (esophageal varices) can rupture, causing life-threatening bleeding that demands urgent intervention.
- Hepatic encephalopathy: Toxin buildup in the brain results in confusion, mood changes, and even coma. For nurses, monitoring mental status becomes essential.
Long-Term Complications
- Portal hypertension: Chronic high pressure in the portal vein not only drives ascites but also causes splenomegaly and worsens varices.
- Coagulopathy: Poor clotting due to reduced protein production increases bleeding risk from even minor injuries.
- Malnutrition and muscle wasting: The liver’s failure to process nutrients contributes to weakness and vulnerability to infection.
- Hepatocellular carcinoma (HCC): Patients with cirrhosis face a higher risk of developing primary liver cancer, requiring lifelong surveillance.
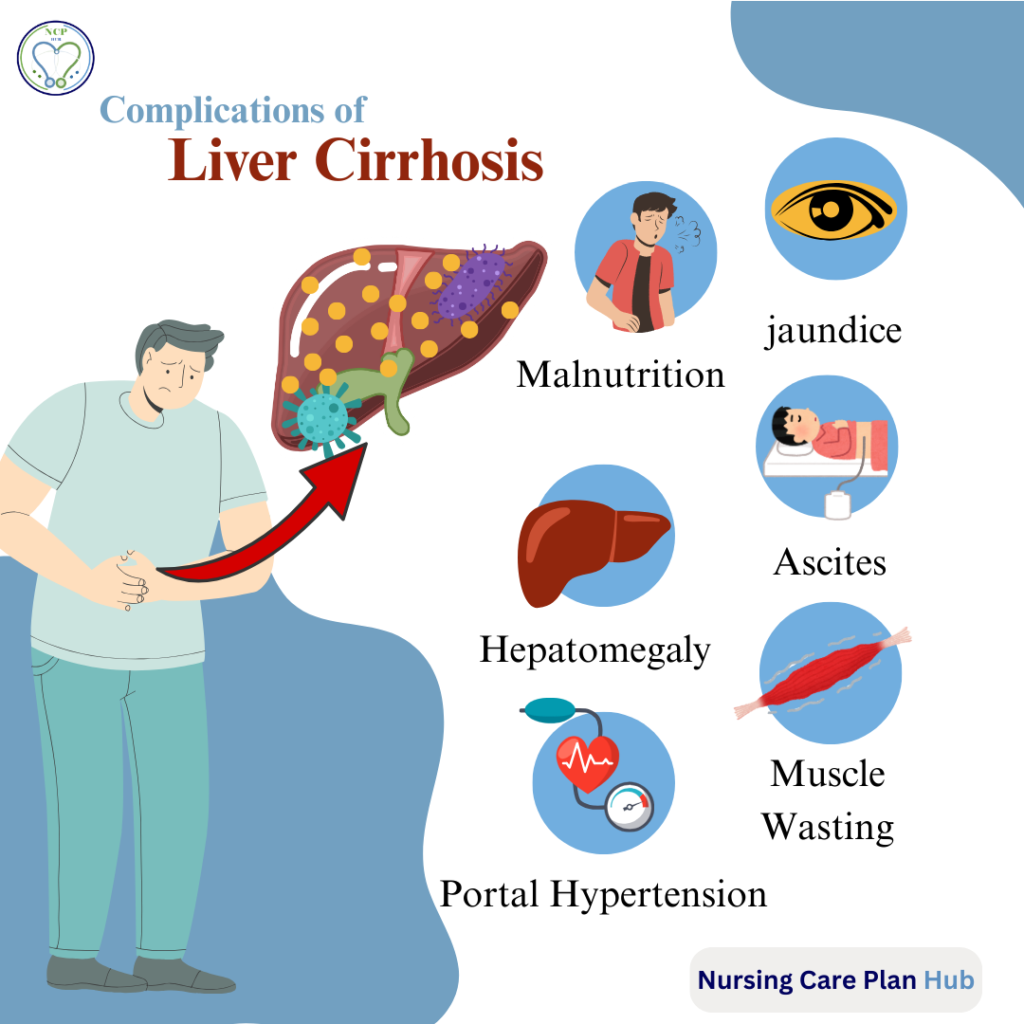
These complications shift cirrhosis from a manageable condition to a life-limiting illness. Daily life is disrupted by fatigue, hospital admissions, and dietary restrictions. For nurses and caregivers, care becomes centered on symptom control, preventing complications, and maintaining dignity. The prognosis often depends on how well these issues are managed alongside the underlying disease.
Diagnostic Findings & Investigations
Diagnosing cirrhosis relies on a mix of lab tests, imaging studies, and bedside assessments. In Mr. K.’s case, these tools confirmed not only the presence of chronic liver damage but also its complications.
Laboratory tests showed elevated liver enzymes (AST/ALT) reflecting ongoing liver injury, alongside low albumin (2.5 g/dL) and prolonged INR (1.9), both pointing to impaired liver function and coagulopathy. A high bilirubin level (4.0 mg/dL) explained his jaundice, while low platelets suggested portal hypertension.
Imaging with abdominal ultrasound revealed a shrunken, nodular liver—a hallmark of cirrhosis—plus splenomegaly and moderate ascites. These features confirmed long-standing structural changes.
Endoscopy detected Grade II esophageal varices, a dangerous complication of portal hypertension.
Clinical assessment findings such as jaundice, hepatomegaly, ascites, and confusion further supported the diagnosis of decompensated cirrhosis.
Together, these results not only establish cirrhosis but also help clinicians stage the disease, monitor progression, and tailor management—whether that means addressing ascites, preventing variceal bleeding, or monitoring for hepatic encephalopathy and liver cancer.
Liver Cirrhosis Nursing Diagnoses
Nursing diagnoses help guide care by identifying patient needs and prioritizing interventions. For a patient like Mr. K. with decompensated liver cirrhosis, several nursing concerns are highly relevant:
Primary Nursing Diagnoses
- Excess Fluid Volume related to impaired liver function and portal hypertension as evidenced by abdominal swelling (ascites), peripheral edema, and breathlessness.
- Impaired Gas Exchange related to abdominal distension limiting diaphragmatic expansion as evidenced by breathlessness and reduced tolerance to activity.
- Imbalanced Nutrition: Less Than Body Requirements related to early satiety, anorexia, and impaired metabolism as evidenced by loss of appetite, fatigue, and poor energy levels.
- Activity Intolerance related to fatigue and dyspnea as evidenced by reduced physical activity and inability to perform daily tasks.
- Fatigue related to chronic illness and decreased metabolic function as evidenced by reduced energy, sedentary lifestyle, and inability to sustain activity.
Secondary / Psychosocial Nursing Diagnoses
- Disturbed Body Image related to abdominal distension, jaundice, and edema as evidenced by visible physical changes and possible embarrassment or social withdrawal.
- Ineffective Health Management related to history of poor compliance with hepatitis C treatment and alcohol use as evidenced by progression of liver disease.
- Risk for Bleeding related to impaired liver function and possible coagulopathy (common in advanced liver disease).
- Risk for Infection related to ascitic fluid accumulation and compromised immunity.
- Deficient Knowledge related to disease process, lifestyle modifications, and treatment regimen as evidenced by history of poor follow-up and late hospital presentation.
These nursing diagnoses provide a roadmap for individualized care, while also serving as entry points for detailed Nursing Care Plans (NCPs) that address each problem in depth.
Liver Cirrhosis Management
Managing liver cirrhosis requires a combination of medical interventions, supportive care, and patient education. The primary goals are to slow disease progression, prevent complications, and maintain quality of life.
Liver Cirrhosis Medical management
Medical management often includes medications to reduce portal hypertension, control fluid retention (diuretics), and manage hepatic encephalopathy (lactulose or rifaximin). In cases of significant ascites, procedures like paracentesis may be performed to relieve discomfort and improve breathing. Screening for esophageal varices and hepatocellular carcinoma is essential, as early detection can prevent life-threatening complications.
Liver Cirrhosis Nursing Care
Nursing care focuses on monitoring symptoms, supporting daily needs, and educating patients and families. Nurses track vital signs, fluid balance, neurological status, and signs of infection or bleeding. They assist with nutrition, provide comfort measures, and encourage mobility while respecting fatigue limitations. Emotional support is equally important, as chronic illness often brings anxiety or depression.
Patient education is central: teaching about alcohol avoidance, medication adherence, dietary modifications, and the importance of follow-up care helps patients participate actively in their own recovery.
By combining medical treatment with attentive, holistic nursing care, patients like Mr. K. can experience improved symptom control, reduced complications, and better overall well-being. Individual Nursing Care Plans (NCPs) then provide step-by-step guidance for addressing each specific nursing diagnosis.
Patient case files are invaluable tools in healthcare. They not only document the patient’s journey but also guide nursing interventions, support medical decisions, and serve as real-world learning resources for students. By organizing key details—demographics, history, lab results, and complications—these records make complex conditions like liver cirrhosis easier to understand and manage.
For nurses, this structured approach ensures each patient receives individualized, holistic care. Students can study cases to strengthen clinical reasoning, while general readers gain insights into disease progression and management.
To explore practical applications, check out our linked Nursing Care Plans (NCPs) for each diagnosis, including Ineffective Airway Clearance, Excess Fluid Volume, and Imbalanced Nutrition. These guides provide step-by-step care strategies and deepen your understanding of liver cirrhosis management.

Very good work… Keep it up